References
Alzheimer's disease hypotheses
Abstract
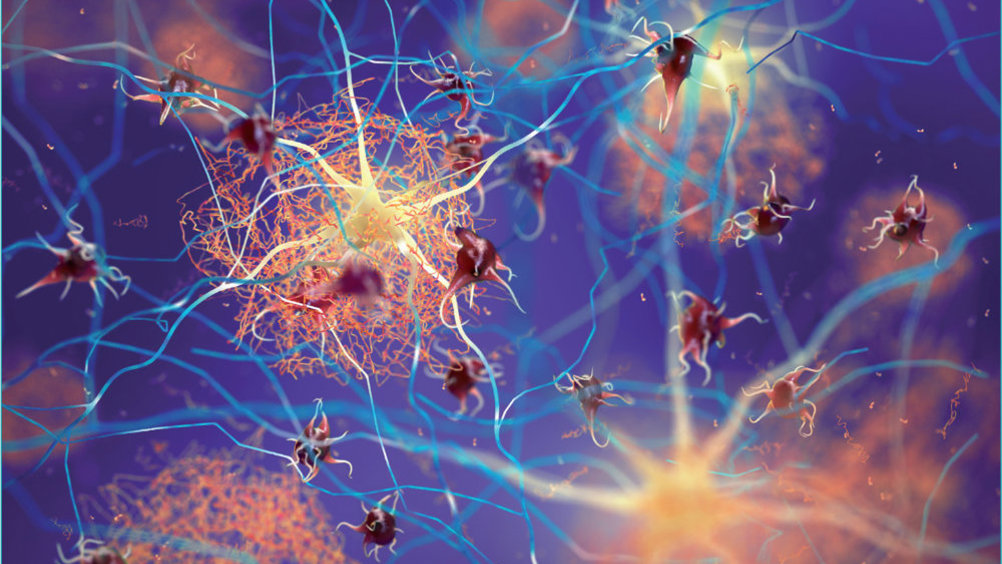
Current work on Alzheimer's disease shows that there is no shortage of hypotheses-generating research attesting to a will to understand, says George Winter
Castillo (2013) notes that the term ‘hypothesis’ is often confused with ‘theory’, explaining that ‘[a] theory is the end result of a previously tested hypothesis, meaning a proved set of principles that explain observed phenomena.’ But he also advises that many consider the scientific method as ‘rigid and constrained in its design and produces results that are isolated from real environments and that only address specific issues.’ So perhaps, as Castillo (2013) posits, there is room for serendipity and an awareness that science is ‘a dynamic process engaging many individuals and activities’ and that data may not always fit into organised and neat conclusions: ‘Science is about discovery, not the justifications it seems to emphasise.’
If nothing else, Castillo's assertions in relation to the scientific method should remind us that, as the historian Marc Bloch put it: ‘The nature of our intelligence is such that it is stimulated far less by the will to know than by the will to understand’ (James, 2007). In this respect, current work on Alzheimer's disease (AD) shows that there is no shortage of hypotheses-generating research attesting to a will to understand.
Register now to continue reading
Thank you for visiting Journal of Prescribing Practice and reading some of our peer-reviewed resources for prescribing professionals. To read more, please register today. You’ll enjoy the following great benefits:
What's included
-
Limited access to our clinical or professional articles
-
New content and clinical newsletter updates each month

