Demands on access to primary care are increasing with the rising prevalence of long-term conditions, multi-morbidity and the effects of COVID-19 (Greenhalgh et al, 2020; Julia et al, 2020; Pettigrew et al, 2020). Medicines use is increasing; with 1 in 4 adults in UK primary care taking five or more medicines daily, there is a need to workforce plan in order to meet prescribing needs (Avery et al, 2012). Thus, mobilising the primary care workforce, including non-medical advanced practice health professionals, is important to address UK primary care prescribing and medicines optimisation needs (Fittock, 2010).
Independent prescribing by non-medical staff, including physiotherapists, is a feature in many UK primary and community care services (Carey et al, 2017), which has many documented benefits including an increase in practitioner autonomy/expertise, enhancement of clinical outcomes compared with doctor-led care (Weeks et al, 2016) and high service user satisfaction (Carey et al, 2017). In Northern Ireland (NI), the number of healthcare practitioners who are eligible to prescribe continues to increase each year.
There are currently approximately 129 physiotherapists registered as non-medical prescribers employed across all Health and Social Care (HSC) Trusts, in respiratory, musculoskeletal (MSK) and lymphoedema specialisms. Fifty-two of those are in first contact physiotherapist roles (with 77 non-first contact physiotherapists) (Weeks et al, 2016).
Despite the benefits of independent prescribing, difficulties with implementation are frequently cited. Reported barriers to adoption have included varying legislative/jurisdictional levels of prescribing autonomy and/or prescribing in heterogeneous care settings (Carey et al, 2020; Department of Health 2023). In NI, some prescribers working at interfaces between primary and secondary care cannot prescribe treatments directly to their patients.
With the exception of first contact physiotherapists working in General Practice (GP) Federation multidisciplinary teams, there is currently no mechanism for prescribers to issue a health service prescription (known as a HS21) directly to the patient. Recommendations made by these specialists have to be implemented by a GP, often causing duplication of effort and delays in treatment.
Understanding and overcoming the barriers to implementation is crucial to fully enable prescribing physiotherapists to use their enhanced skills, to empower the profession and ultimately improve patient care (Jebara et al, 2018; Mills et al, 2021; Edwards et al, 2022). In NI, a new model of prescribing (NMOP) was proposed to address these challenges and enable prescribers to work at the interface in a more effective and autonomous way.
Aim
To develop and deliver a NMOP pilot with physiotherapists prescribing, in community and outpatient settings in NI HSC. The specific objectives of the project were to:
Methods
A NMOP was developed by a Task and Finish group involving the HSC Board, Public Health Agency, HSC Trusts and GPs. The Task and Finish group involved extensive stakeholder engagement to define the key principles of the model and scope out the arrangements that needed to be in place. The agreed NMOP facilitated issuing of HS21 prescription forms by a qualified physiotherapist prescriber in the specialities of respiratory, lymphoedema, MSK, women's health and neurology.
Prescribing was permitted where there was an urgent need for medication (within 72 hours of consultation), a requirement for titration/tapering of medicines with early review, or a need for specialised items outside the clinical expertise of a GP. The model involved deployment of digital communication systems via electronic treatment advice notes (eTAN) to GP practices. The Task and Finish group met regularly throughout the pilot to facilitate quality assurance and to identify and resolve any issues with service design and delivery.
Outcome measures
Analysis
Data on medicines prescribed, deprescribed and changed was audited for a 1-week period at the start (16/11/2020) and end (30/06/2021) of the pilot. Audit activity was collated using Microsoft Excel. Data was quality checked and re-categorised as necessary. Descriptive statistics were used to summarise activity at the start and end of the pilot and results were tabulated.
Process maps and patient journeys were recorded and tabulated. Steps and time taken were summarised. Qualitative responses from clinician surveys were themed and reported. Descriptive statistics were used to summarise results from patient satisfaction survey responses.
Results
Audit
Prescribing activity
Between November 2020 and June 2021, 19 physiotherapy prescribers in the Southern HSC Trust and South Eastern HSC Trust were involved. Clinicians were invited to submit activity from 1 week of their practice from before the start of the pilot (16/11/2020) and at the end of the pilot (30/06/2021). Data are summarised in Table 1. There was little change in the prescribers' locality, years of prescribing experience or proportion of time dedicated to clinical activities. There was an increase in the ability of prescribers to facilitate face-to-face consultations at the end of the pilot due to a relaxation in COVID-19 pandemic restrictions. There were also a greater proportion of prescribers working in respiratory compared with MSK, reflecting the opportunities to prescribe in an acute situation.
| Start | End | |
|---|---|---|
| Number of prescribers recording data | 16 | 15 |
| Number of patient contacts | 148 | 82 |
| Prescriber background n (%) | ||
| Respiratory | 52/148 (35%) | 32/82 (39%) |
| ICATS | 46/148 (31%) | 3/82 (4%) |
| Lymphoedema | 18/148 (12%) | 27/82 (33%) |
| Muskuloskeletal | 18/148 (12%) | 0/82 (0%) |
| ICT physiotherapy | 9/148 (6%) | 6/82 (7%) |
| CST | 3/148 (2%) | 2/82 (2%) |
| Neurology | 2/148 (1%) | 5/82 (6%) |
| Mean working time equivalent clinical time | 0.7 *n=14/16 | 0.7 *n=11/15 |
| Mean number of years qualified as prescriber | 2.8 *n=8/16 | 2.7 *n=9/15 |
| Trust | ||
| SHSCT | 90/148 (61%) | 49/82 (60%) |
| SEHSCT | 58/148 (39%) | 33/82 (40%) |
| Patient diagnosis n (%) | ||
| Exacerbation of chronic respiratory condition | 29/148 (20%) | 26/82 (32%) |
| Neck and back pain | 25/148 (17%) | 1/82 (1%) |
| Limb pain | 18/148 (12%) | 0/82 (0%) |
| Lymphoedema | 18/148 (12%) | 27/82 (33%) |
| Arthritis/tendonitis | 17/148 (11%) | 2/82 (2%) |
| Neurological condition | 12/148 (8%) | 11/82 (13%) |
| Acute respiratory condition | 10/148 (7%) | 3/82 (4%) |
| Other | 10/148 (7%) | 4/82 (5%) |
| UTI | 5/148 (3%) | 5/82 (6%) |
| Other respiratory condition | 3/148 (2%) | 3/82 (4%) |
| Diabetes | 1/148 (1%) | 0/82 (0%) |
| Consultation n (%) | ||
| Virtual | 54/145 (37%) | 16/82 (20%) |
| Face to face | 76/145 (52%) | 66/82 (80%) |
| Not reported | 15/145 (10%) | 0/69 (0%) |
ICATS: Integrated Clinical Assessment and Treatment Services; CST: Community Services Team; ICT: Integrated Community Team; UTI: Urinary Tract Infection
When comparing activity at the start and at the end of the audit, the proportion of patient consultations where a medication or garment was changed (started, stopped, or both) was greater at the end of the pilot (Table 2).
| n (%) | Baseline |
Final |
Change from start to end of audit |
|---|---|---|---|
| Item started | 50/148 (34%) | 51/82 (62%) | ↑ |
| Item stopped | 6/148 (4%) | 4/82 (5%) | ↑ |
| Item started and stopped | 6/148 (4%) | 8/82 (10%) | ↑ |
| Not reported | 1/148 (1%) | 0/82 (0%) | ↓ |
| Recording no change to item | 85/148 (57%) | 19/82 (23%) | ↓ |
Overall, at baseline there were 62/148 patients, and at the end of the audit there were 63/82 patients; where medication or garment was changed (stopped, started or both). The mechanism used to generate the prescriptions is detailed in Table 3. At baseline, most changes to medication or garment were initiated by either letter of recommendation, telephone call or email or both, requiring GP resource to follow up and prescribe the medication/garment. With the introduction of the NMOP, this decreased. At the end of the pilot, 79% (50/63) of items were prescribed using HS21 or a combination of HS21 plus another method, removing the need for GP to action.
| LOR | TC/email | LOR plus TC/email | HS21 | HS21 plus LOR | HS21 plus TC/email | HS21 plus LOR plus TC/email | Not reported | Total | |
|---|---|---|---|---|---|---|---|---|---|
| Baseline | 31/62 (50%) | 3/62 (5%) | 13/62 (21%) | 6/62 (10%) | 62/62 (100%) | ||||
| Final | 6/63 (10%) | 0/63 (0%) | 1/63 (2%) | 41/63 (65%) | 2/63 (3%) | 3/63 (5%) | 4/63 (6%) | 0/63 (0%) | 6/63 (100%) |
| Change from start to end of audit | ↓ | ↓ | ↓ | ↑ | ↑ | ↑ | ↑ | ↓ |
LOR: Letter of recommendation; TC/email: Telephone contact or email contact with GP; Other action: Other action (completion of hospital paperwork (Kardex or HOOF)
Prescribing compliance
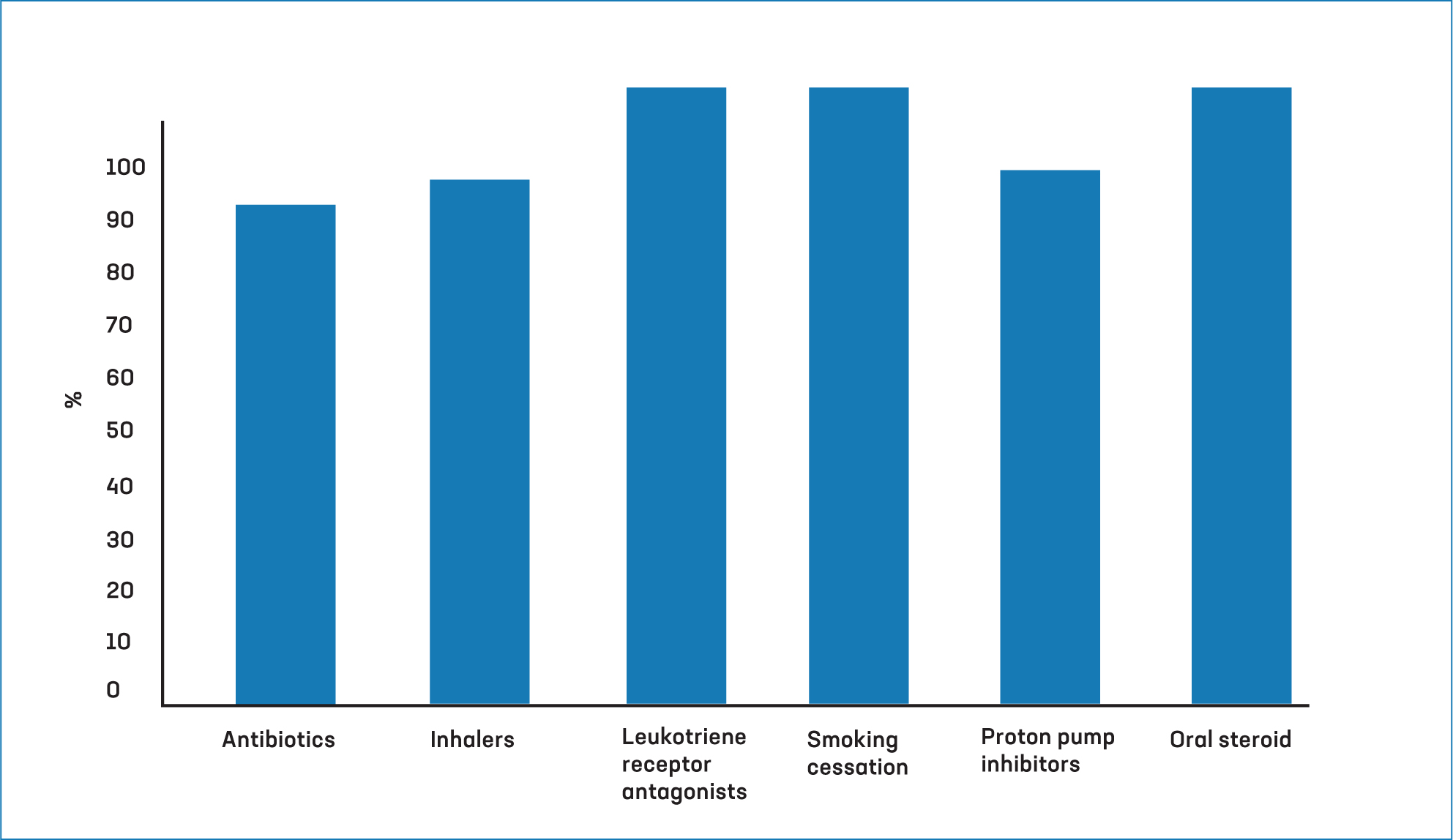
In all therapeutic areas, the prescribers exceeded 70% compliance with NI Formulary choices (range 81% to 100% compliance) indicating that prescribing activity as part of the pilot was evidence based (Figure 1).
Process maps and patient journeys
Table 4 summarises the process maps of the clinical pathway of prescribing at the start and end of the pilot. They showed a reduction in both the number of steps and the time taken in all service areas.
| Specialty | Number of steps/times at start of NMOP pilot | Number of steps/time at end of NMOP pilot | Number of steps/time |
|---|---|---|---|
| Lymphoedema | 9 steps |
Supply via *DAC: 6 steps |
↓ |
| Musculoskeletal | 8 steps |
7 steps |
↓ |
| Respiratory outpatients | 10 steps |
7 steps |
↓ |
| Respiratory – acute care at home | 7 steps |
5 steps |
↓ |
| Orthopaedic ICATS | 8 stepsaTotal timescale: 1–7 days | 7 steps |
↓ |
On average, the number of steps required reduced by two. Positive impacts were documented in the patient journeys (Table 5) in the respiratory and lymphoedema clinical pathways, including increased patient convenience, time savings and improved prescription access, among others. The patient journey in the ICATS clinical pathway documented the limitations of implementing the NMOP pilot practices.
| Clinical area | Key findings |
|---|---|
| Respiratory | NMOP: |
| Lymphoedema | NMOP: |
| ICATS |
|
Stakeholder session and surveys
Physiotherapist and GP perspectives
Key themes were identified from the stakeholder feedback session (involving 24 stakeholders) in relation to the benefits, challenges and requirements for regional roll-out. Themes generated were linked to aspects of communication, training and governance processes. Other areas impacted by stakeholders included staff training, collaboration, impact of COVID-19, prescribing criteria, policy guidance, funding and paperwork. Forty-six stakeholder survey responses were obtained from physiotherapists (16/46; 35%), GPs, (14/46; 30%) and pharmacists (13/46; 28%) or other stakeholders (3/46; 7%). Responses addressed a number of areas as follows.
Benefits
The majority of respondents (37/46; 80%) felt that physiotherapy NMOP benefited the patient. Benefits included a reduction in the delay in accessing urgent medicines, a reduction in the risk of inappropriate medicines/appliances being prescribed and errors, a reduction in the burden on GP practices, increased convenience for patients, more streamlined processes, improved patient access to specialist clinician and better provision of medicines information about medications. Other benefits for the clinician and the clinical pathway were reported by 35/46 (76%) of respondents including safer prescribing due to less need for transcription, faster access to medicines, provision of support to GPs during COVID-19 pandemic, increased efficiency and optimisation of skills.
Challenges
Thirty-five out of 46 (76%) stakeholders responded indicating that they had not come across any challenges. Of those reported, key themes included additional administration time associated with data collection to support evaluation of the project, limitations to prescribing ability due to use of compliance aids, medicines legislation, delays in allocating cipher numbers to prescribers and establishing electronic communication with GP practices. It was also difficult to secure community pharmacy representation for the Task and Finish Group. One respondent highlighted that because this pathway was still ‘niche’ and not widespread across the region it would be difficult to raise awareness among other stakeholders that this was now a possibility.
Improvements for full implementation
Twenty-eight out of 46 stakeholders (61%) suggested improvements (Box 1), including the need for a regionally commissioned service to ensure adequate resource, the importance of access to digital technology to enable remote access to appropriate records and decision support software, and clear departmental policy to support this model of care. Most respondents (38/46; 83%) indicated that they were happy for NMOP to continue.
Key themes highlighted how respondents wanted the service to be commissioned and streamlined into business as usual. GP respondents were keen to understand how this new approach to prescribing reduced their workload. Trust pharmacists wanted assurances that the prescribing would continue to be funded and monitored as per the processes established for the pilot project.
Physiotherapists involved acknowledged that they had received good support across the multidisciplinary team in establishing this new pathway. However, MSK physiotherapists felt that the opportunity for them to prescribe was limited due to current controlled drug legislation for physiotherapists and the NMOP project criteria with which they could write a HS21 prescription.
Patient satisfaction survey
Sixty-four patient survey responses were collected and a large majority of patients agreed that they were aware of, clearly advised and informed during the NMOP process and were satisfied with the service (Table 6). However, in the instances where no medications/garments were prescribed, but there were changes to existing medications/garments, fewer patients were aware. Overall, patients reported a wide range of benefits (Figure 2).
| Statement | % agree | % disagree | % not answered |
|---|---|---|---|
| 1. I was aware the medication/garment was being prescribed/reviewed by a physiotherapist prescriber (n=63) | 95% | 3% | 2% |
| 2. It was explained clearly why the medication/garment was prescribed (n=63) | 97% | 3% | |
| 3. I was advised on how to take the medication and how long to take the medication for (n=43) | 100% | ||
| 4. I was advised of possible risks or side effects and what to do should there be any reaction to the new medication prescribed (n=43) | 98% | 2% | |
| 5. I was informed of arrangements to obtain repeat prescriptions (n=43) | 98% | 2% | |
| 6. I was advised on how to correctly apply the garment and how long to wear (n=20) | 100% | ||
| 7. I was advised of possible risks or side effects and what to do should there be any reaction to the new garments being issued (n=20) | 95% | 5% | |
| 8. I was informed of arrangements to obtain repeat prescriptions (n=20) | 95% | 5% | |
| 9. I was satisfied with the consultation and felt I received appropriate and sufficient information (n=62) | 97% | 3% | |
| 11. If there were no medications/garments prescribed, but there were changes to my existing medications/garments, I was aware of future planned changes (n=64) | 27% | 27% | 47% |

Discussion
In this evaluation, the audit and survey activity clearly showed benefits for patients, clinicians and service delivery across a range of clinical areas. There was an increase in the delivery of prescriptions using the NMOP mechanisms and a reduction in the use of letter of referral, telephone call or email mechanisms for prescription, removing the need for a GP to action. In all therapeutic areas involved, prescribing was evidence based as per the NI formulary. Following the introduction of the NMOP, there was a reduction in both the number of steps and the time taken in all service areas.
The majority of physiotherapists involved in the pilot reported clear benefits to patients, notably reducing prescription delays, reducing risk of inappropriate prescriptions and providing access to specialist clinicians. Physiotherapists also reported clear benefits for clinicians, including more efficient processes and the optimisation of the NMP skills and patients reported high levels of satisfaction with a wide range of benefits.
What improvements/considerations should be made for full implementation? Key findings
The positive findings from this NMOP pilot project align with a range of facilitators to NMP which have been outlined previously including impacts on patient care, clinicians' prescribing role and practical aspects (Graham-Clarke et al, 2022). The efficiency and quality findings from the NMOP practices in this project add to the wider body of evidence supporting NMP, including improvements in a range of safety and patient-reported outcome measures (Noblet et al, 2018).
Several studies have underlined that a coordinated, collaborative and inclusive approach across systems levels is essential for non-medical prescribing to be fully implemented (Noblet et al, 2017; Stewart et al, 2017; Graham-Clarke et al, 2022). In agreement with the literature, collaborative working and collective leadership involving a multidisciplinary task and finish group was key to the implementation of the project.
This project identified the constraints of the new prescribing process and identified aspects that would require further consideration before any further roll-out of the new model. In one clinical area, MSK physiotherapists could not fully engage in the NMOP due to a limited ability to prescribe controlled drugs as regulated by the Misuse of Drugs legislation and the nature of many MSK ailments (acute phase had been managed with medication between referral and consultation).
This finding highlighted that scoping the feasibility of any newly proposed NMOP to meet at least one of the three permitted criteria and ability to meet governance requirements, is important for further roll-out. Other barriers highlighted by clinicians included additional paperwork and the time required to compile new advice notes, issues with receiving treatment advice notes and despite implementation of a communication strategy, challenges with engaging all GPs across the Trust localities. As the literature underlines, the importance of medical professionals' support in enabling non-medical prescribing is key area for continued success and will require ongoing stakeholder engagement (Graham-Clarke et al, 2021).
Conclusion
In this project, a multidisciplinary Task and Finish Group was successful in collaborating to develop a quality assured NMOP programme for physiotherapists, which delivered integrated care tailored to individual patient requirements.
A range of favourable outcomes with the NMOP for physiotherapists was described through audit and survey, including benefits to the patient, HSC system and the clinicians involved. Importantly, challenges identified areas for future learning and improvement. The successes of the project resulted in the integration of NMOP into business as usual across participating Trusts for certain physiotherapy specialties. The experience of this NMOP project can serve as an example of the capacity and commitment required to deliver a NMOP in other patient service pathways.


