In 2020, the COVID-19 pandemic dramatically reshaped primary care service delivery through increased remote consultation to reduce viral transmission. A systematic review of the evidence of its impact on antibiotic prescribing behaviour by Han et al (2020) was inconclusive. The studies included in Han et al's (2020) were conducted prior to the pandemic and the risk/benefit analysis of face-to-face consultations and the willingness and ability of both patients and clinicians to engage in them were very different, which may have influenced prescribing decisions.
Demonstrating the differences in prescribing patterns in 2020, compared to the preceding 4 years, will help understand whether non-medical prescribers (NMPs) were affected differently, compared to their medical colleagues in terms of their antibiotic prescribing when the majority of primary care consulting was moved to remote patient interactions. For the present study, changes in prescribing patterns as a result of the COVID-19 pandemic were analysed to identify any shifts in behaviour and how this may have affected the antimicrobial stewardship (AMS) of NMPs.
Methods
Prescribing data for antibiotics prescribed by NMPs in primary care and dispensed in the community was obtained from NHS Business Services Authority and the regulating bodies for the professions with non-medical prescribers via Freedom of Information requests and was standardised using mid-year population estimates from the Office for National Statistics. Details of exact requests available in part 1 (Brett and Palmer, 2022). Comparisons were made between the antibiotic prescribing that occurred after the first quarter of 2020 with the preceding years and changes in prescribing patterns as a result of the COVID-19 pandemic were analysed to identify any shifts in behaviour and how this may have affected the AMS of NMPs.
Results
The proportions of dispensed antibiotics per 100 000 population prescribed by medical and NMPs remained stable at 89% and 11%, respectively, in 2019 and 2020. There was a 12% drop in the total volume of dispensed antibiotic items per 100 000 population prescribed by NMPs between 2019 and 2020 (Table 1).
Table 1. Antibiotic prescribing data for NMPs in primary care in England 2016-2021
| 2016 | 2017 | 2018 | 2019 | 2020 | |
|---|---|---|---|---|---|
| Total prescription items written by NMPs | 28248175 | 3266782 | 39107085 | 48258784 | 60445390 |
| Total antibiotic prescription items written by NMPs | 2866437 | 2844502 | 2943516 | 3105064 | 2746283 |
| Antibiotic prescription items per 100 000 population written by NMPs | 5186.42 | 5114.23 | 5258.42 | 5516.49 | 4856.38 |
| Percentage of all antibiotic prescription items written by NMPs | 10.63% | 9.02% | 9.76% | 10.55% | 10.59% |
| Percentage of NMP prescriptions that were for antibiotics | 10.15% | 8.71% | 7.53% | 6.43% | 4.54% |
| Total high-risk antibiotic prescription items written by NMPs | 149484 | 149472 | 155074 | 164021 | 175283 |
| High-risk antibiotic prescription items per 100 000 population | 270.47 | 268.74 | 277.03 | 291.40 | 309.96 |
| Percentage of high-risk antibiotic prescriptions written by NMPs | 5.21% | 5.25% | 5.27% | 5.28% | 6.38% |
This followed a general trend of annual increases apart from a 1.4% drop in 2017. Nurses and physiotherapists demonstrated a considerable reduction in total antibiotic items prescribed between 2019 and 2020 (by 16% and 34%, respectively). Conversely, the other professions had continued increases, with paramedic prescribing increasing by 277% (Table 2).
Table 2. Total antibiotic items prescribed by NMPs in England and dispensed in the Community by profession and year
| Profession | Total dispensed antibiotics by profession (%) | ||||
|---|---|---|---|---|---|
| 2016 | 2017 | 2018 | 2019 | 2020 | |
| Nurse | 2797523 (97.6) | 2738801 (96.3) | 2783497 (94.6) | 2869798 (92.4) | 2421975 (88.2) |
| Pharmacist | 55259 (1.9) | 98388 (3.5) | 154246 (5.2) | 218137 (7.0) | 280219 (10.2) |
| Optometrist | 16 (0.0) | 42 (0.0) | 35 (0.0) | 45 (0.0) | 62 (0.0) |
| Paramedic | 0 (0.0) | 0 (0.0) | 0 (0.0) | 9,962 (0.3) | 37 557 (1.4) |
| Physiotherapist | 300 (0.0) | 568 (0.0) | 1487 (0.1) | 2752 (0.1) | 1829 (0.1) |
| Podiatrist/chiropodist | 1976 (0.1) | 3062 (0.1) | 3857 (0.1) | 3992 (0.1) | 4413 (0.2) |
| Community nurse | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 4 (0.0) |
| Unidentified prescriber | 11363 (0.4) | 3641 (0.1) | 394 (0.0) | 378 (0.0) | 217 (0.0) |
The total high-risk antibiotics (co-amoxiclav, cephalosporins and quinolones) prescribed per 100 000 population continued to rise (from 291 to 310), despite the overall drop in antibiotic prescribing in 2020. The percentage of high-risk antibiotics prescribed rose from 5.3% in 2019 to 6.4% in 2020. In contrast, from 2016 to 2019, high-risk antibiotic prescribing by NMPs increased only very slightly—from 5.2% to 5.3% of all antibiotics prescribed (Table 3).
Table 3. Dispensed high-risk antibiotics (co-amoxiclav, cephalosporins and quinolones) prescribed in Primary care as a percentage of the total antibiotics prescribed by medical and NMPs 2016-2021
| Prescriber type | Total high-risk antibiotics dispensed per 100 000 population | Total antibiotics dispensed per 100 000 population | Percentage high risk to total | |
|---|---|---|---|---|
| 2016 | Medical | 3614.18* | 43 594.18* | 8.29%* |
| NMP | 270.49 | 5186.42 | 5.22% | |
| Total | 3884.65* | 48 780.53* | 7.96%* | |
| 2017 | Medical | 4670.89 | 51 611.31 | 9.05% |
| NMP | 268.74 | 5114.23 | 5.25% | |
| Total | 4939.75 | 56 725.17 | 8.71% | |
| 2018 | Medical | 4372.41 | 48 615.19 | 8.99% |
| NMP | 277.03 | 5258.42 | 5.27% | |
| Total | 4649.42 | 53 873.44 | 8.63% | |
| 2019 | Medical | 3986.27 | 46 768.29 | 8.52% |
| NMP | 291.40 | 5516.49 | 5.28% | |
| Total | 4277.67 | 52 284.77 | 8.18% | |
| 2020 | Medical | 3931.63 | 40 989.95 | 9.59% |
| NMP | 309.96 | 4856.38 | 6.38% | |
| Total | 4241.59 | 45 846.33 | 9.25% |
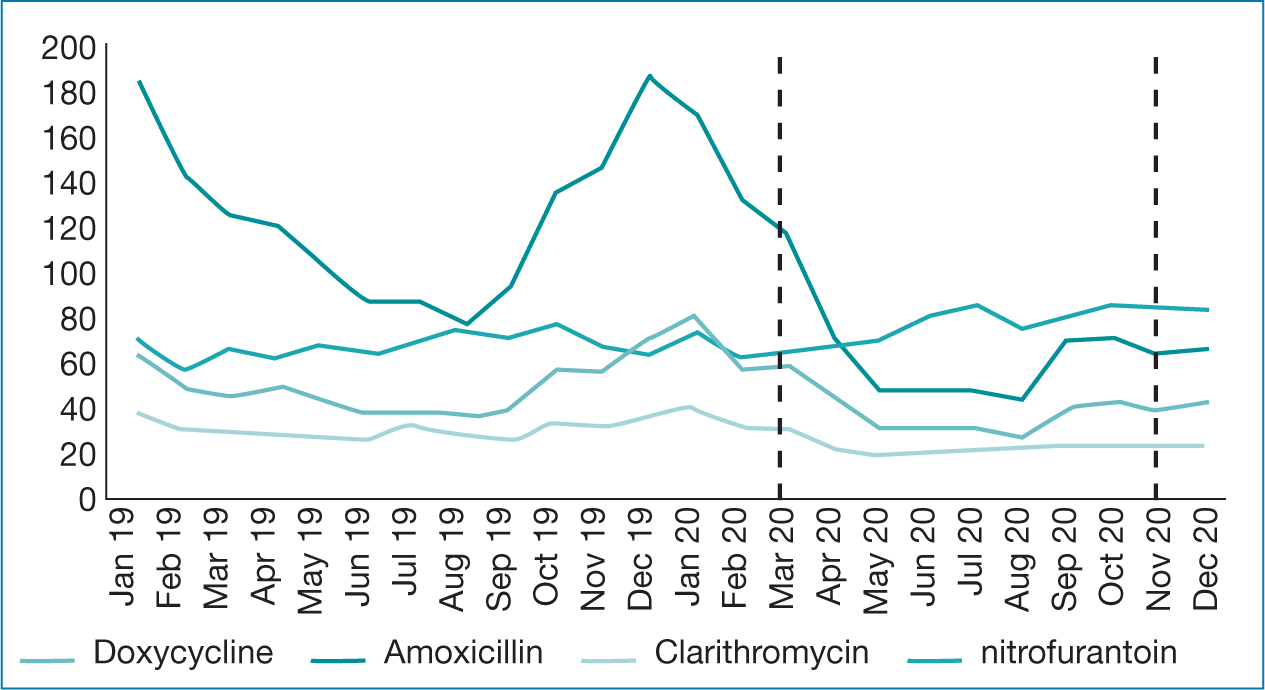
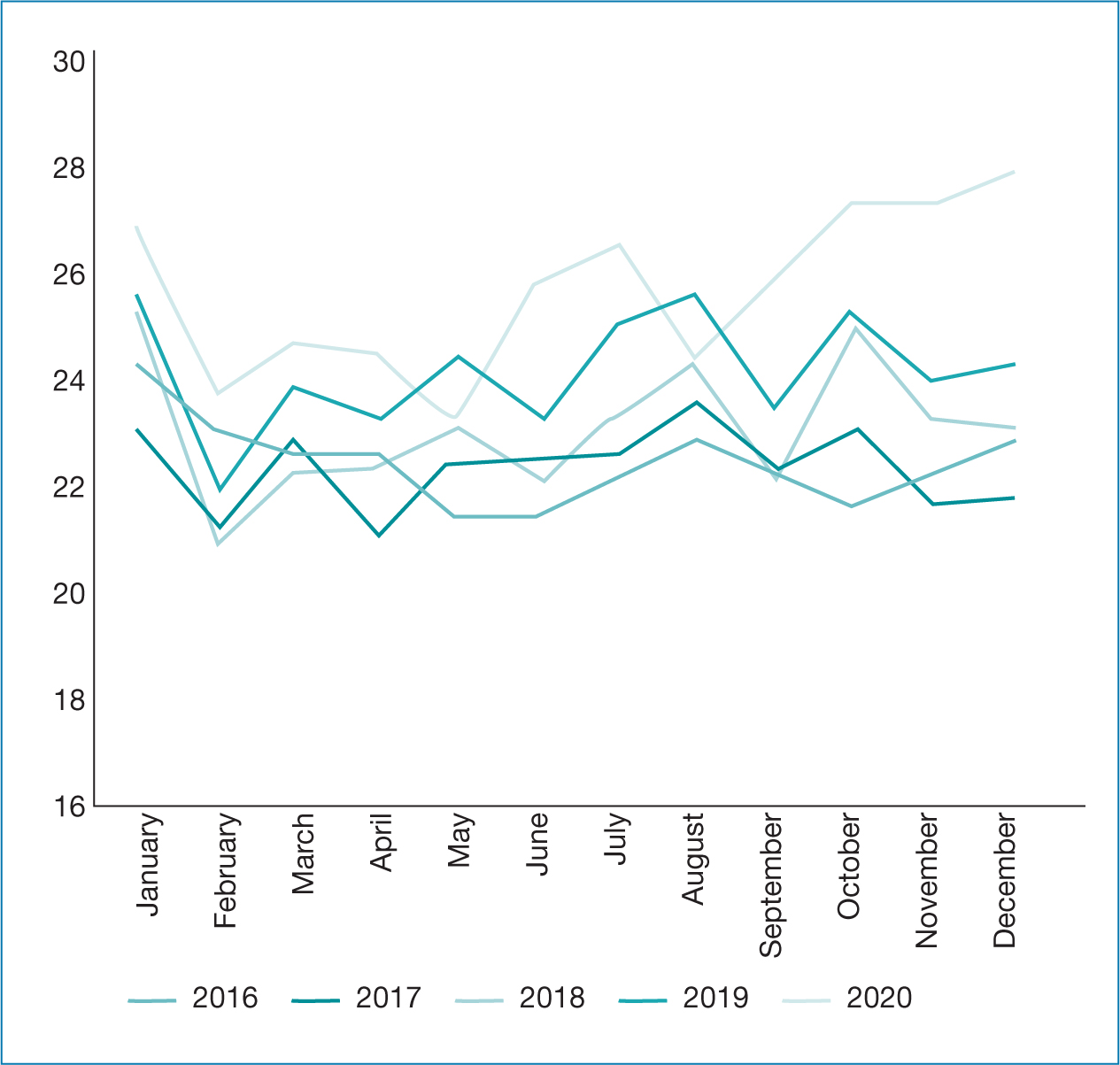
The seasonal patterns of prescribing slightly differed in 2020, with the summer peak occurring in July and August 2016–2019, but arriving a month earlier, and dipping in August rather than September. In 2020, there was then a sustained rise in high-risk prescriptions, which levelled out from September to October and then rose steadily until December, without any of the October/November decreases previously observed in 2016–2019 (Figure 2).
Discussion
Prescribing during the COVID-19 pandemic was challenging; therefore, an impact on antibiotic prescribing patterns was expected (Andrews et al, 2021). Making conusltations remote from March 20220 resulted in a rapid recudction of COVID-19 (Majeed et al, 2020). The evidence surrounding remote consultations and their safety and cost-effectiveness was mixed prior to the COVID-19 pandemic (Campbell et al, 2015; Donaghy et al, 2019; Hammersley et al, 2019; Mold et al, 2019). There was particularly limited evidence on the mpact of remote consultation on the prescribing of antibiotics and AMS (Han et al, 2020). A widely acknowledged concern for clinicians regarding remote consultation is the clinical uncertainty presented by the inability to physically examine patients. This issue was intensified during the pandemic, as increasingly complex cases were having to be managed remotely (Murphy et al, 2021). NMPs may also have had little or no experience or training in remote consultation prior to the pandemic, potentially impacting their antibiotic prescribing behaviour.
Qualitative studies appear to support the idea that NMPs are less influenced by non-clinical reasons, such as patient expectations, to prescribe antibiotics (Courtenay et al, 2017a) than medical prescribers, and use guidelines and protocols to support their decisions; however, it has been demonstrated that cases of clinical uncertainty cause concern for NMPs (Rowbotham et al, 2012; Ness et al, 2016; Courtenay et al, 2017; 2019). A recent systematic review using theoretical domains framework identified that fears of missing something, leading to a negative consequence for the patient, affecting NMP prescribing (Chater et al, 2020). This is likely to be heightened in a situation where the patient is remote, as safety compromises exist in both using and not using antibiotics (Boiko et al, 2020). This may be particularly relevant when considering the changes in patterns of prescribing that occurred in 2020.
While overall antibiotic prescribing decreased during 2020, prescribing behaviour varied with antibiotic type. Penicillins showed the biggest reduction in dispensed antibiotics in 2020, broadly aligning with surveillance reports of antibiotic consumption in general practice (Public Health England, 2021). Variations were noticeable particularly in antibiotics commonly used as first line treatment for respiratory tract infection (eg amoxicillin and doxycycline) (Figure 1). These showed a steeper decline in use from March 2020 (the first English national lockdown) than in 2019. These then remained at a lower level through to early summer, increased in September, before dropping below 2019 levels in November (second lockdown) where, in contrast to 2019, they remained low until December. This lower level could have a number of factors: greater awareness that these infections are predominantly viral (Gillies et al, 2021; Malcolm et al, 2020) and strong suspicion of COVID-19, with reports of coughs/fevers; public avoidance of medical services in the initial phases of the pandemic (Dilworth and Brummitt, 2021); social isolation reducing transmission of normally circulating viral infections. Guidelines for treating lower respiratory tracts infections also changed during the pandemic, recommending doxycycline as first-line over amoxicillin when bacterial involvement was suspected in chest infection (National Institute for Health and Care Excellence, 2021). Therefore, the reduction in total antibiotic prescribing by NMPs by 6% over the 5-year period (2016–2020) may have been falsely lowered by changes in prescribing and healthcare seeking behaviours that occurred during the COVID-19 pandemic (Brett and Palmer, 2022). Ongoing monitoring will be required to identify whether this lower level of prescribing is sustained and, if so, what the impact is on patient outcomes. One study has suggested that, while total antibiotic prescribing volume declined significantly in 2020, there was a huge reduction in appointments early in the pandemic and there was actually a significant increase in prescriptions of antibiotics over what might have been expected (Armitage and Nellums, 2020). Over the same period, in-hospital antibiotic prescribing rose (Public Health England, 2021). It is important to establish whether not prescribing may, in some cases, be leading to delayed treatment and sicker patients needing in-hospital treatment. Although this trend could also be explained by changes in hospital populations, with decreased elective admissions and increased numbers of COVID-19 patients requiring intensive care unit or high dependency care.
Conversely, there was a trend of increased use of higher-risk antibiotics during 2020, which has been supported by other studies (Andrews et al, 2021; Zhu et al, 2021). Studies into the influences on NMPs antimicrobial prescribing, both on whether and what to prescribe, suggest that, though national guidelines and the British National Formulary were used to aid these decisions by most NMPs, these professionals were also strongly influenced by patient condition and diagnostic uncertainty (Rowbotham et al, 2012; Ness et al, 2016). Before COVID-19, remote consultations, which make accurate patient assessment more difficult, were more easily followed up with face-to-face appointments, mitigating the risk of inappropriate prescribing. While these pressures were similar for medical prescribers, who also felt that their thresholds for antibiotic prescribing were lower early in the pandemic (Borek et al, 2021), they had routinely used telephone consultation prior to COVID-19. A potential lack of experience and training in this method of consultation among NMPs may have contributed to over-prescribing, as eliciting the information required and building a rapport with the patient requires different communication skills to be developed by the clinician (Roberts and Osborn-Jenkins, 2021).
Additionally, it is possible that those patients in genuine need of broad-spectrum antibiotics, who were potentially more unwell, were still seeking help and getting treatment, whereas those with self-limiting infections may have avoided health services. Without data on appointment numbers and details of individual appointments, there is insufficient evidence to say whether the differences noted were because of AMS issues during the pandemic or changes in patient healthcare-seeking behaviour.
Prescribing of antibiotics for urinary tract infections was higher in 2020 than 2019 and peaked a month earlier, in July rather than August: 2020 levels also failed to decline to the same degree seen in the previous year during November and December. This suggests that there may be more confidence in the empiric treatment of urinary tract infections, and more experience in triaging these over the phone. Additionally, urine samples can be collected, dipped and sent for culture without the patient being present, although incorrect use of urine dipsticks can potentially lead to inappropriate prescribing in these circumstances too, particularly among elderly patients (Shallcross et al, 2020).
Conclusions
The challenges of prescribing during the pandemic appear to have had a more detrimental impact on the rates of high-risk antibiotic prescribing for NMPs than their medical colleagues, highlighting the differences both in influences on prescribing practice and experience and training in remote consultation methods. As higher levels of remote consultation are likely to continue post-pandemic, it is important to monitor trends in both the prescribing of antimicrobials and in outcomes for patients, as both not prescribing (when it might be required) and over-prescribing of high-risk antibiotics have the potential for detrimental patient outcomes and increased admissions to secondary care.
There is a need for further research into how these adapted ways of working can be integrated into AMS programmes and training alongside further investigation into the quality and safety issues that have arisen.
The arrival of a viral respiratory infection in 2020, causing a global pandemic, led to a significant reduction in total antibiotic prescribing, but most notably in prescribing for respiratory infections. While social isolation may have reduced transmission of normal seasonal viruses, it seems likely that these data also illustrate that antibiotics are often over-prescribed for self-limiting viral respiratory tract infections.


