Globally, the COVID-19 pandemic is a priority for every healthcare system. The National Health Service (NHS) was pushed to its limit, necessitating the Government to urge the public to ‘stay home’ and reduce non-urgent contact with the NHS (gov.uk, 2020). Whilst the public dutifully obliged, ill health inevitably continued. Healthcare professionals, including non-medical prescribers (NMPs) needed to assess and treat patients whilst minimising in person contact and footfall in all healthcare settings. This facilitated the rapid implementation of remote consultations (telephone and / or video) and the digitalisation of the NHS.
Similarly, the pandemic forced universities to provide education and assessments virtually. For healthcare programmes such as NMP, the training needed to replicate the unprecedented changes to practice and the adoption of remote consultations, examination and prescribing. In order to maintain patient safety, these changes needed to comply with professional regulations and standards (General Pharmaceutical Council, 2018; Health and Care Professions Council, 2019; Nursing and Midwifery Council, 2019).
The article is divided into two sections. First, the practical and regulatory aspects of remote consultations and patient safety will be discussed. Then the experiences of the NMP academic team and its learners will be explored.
Remote consultations before COVID-19
Before the pandemic, the modernisation of the NHS included digitalisation and the use of remote consultations (NHS UK, 2019; Welsh Government, 2019; NHS Digital, 2020). There had been a slow but steady move towards remote consultations in a variety of settings such as chronic conditions or cardiac device follow up (Fauchier, et al, 2005; Crossley et al, 2011; Flodgren et al, 2015). In primary care, remote consultations were identified as alternatives to in person consultations for some, but not all patients (Downes et al, 2017; Atherton et al, 2018). Their successful implementation was dependent upon the surgeries ability to manage their introduction and change processes (Downes et al, 2017; Atherton et al, 2018).
To ensure patient safety, 13 professional regulators and bodies collaborated and produced a document outlining the principles of best practice for all prescribers using remote consultations and prescribing (GMC et al, 2019). Three months after its publication, the pandemic arrived and the implementation of remote consultations and prescribing was fast tracked both in the UK and globally (Portnoy et al, 2020; Gilbert et al, 2020; Jimenez-Rodriguez et al, 2020; NHS Wales, 2020). Remote consultations eliminated the need to travel to healthcare settings (Raven et al, 2013; Greenhalgh et al, 2016; Powell et al, 2017; Thiyagarajan et al, 2020), which was advantageous in regard to reducing transmission of the virus. Whilst many patients prefer in person consultations (Thiyagarajan et al, 2020), the majority were accepting of remote consultations (telephone or video) during the pandemic (Locke et al, 2020).
Remote consultations during the pandemic
Many services used telephone consultations as a ‘first line’ assessment to risk assess individual patients' needs (Al Hasani et al, 2020). From a governance perspective, it is important to ensure that the professional undertaking this assessment is suitably trained and experienced. This is because their clinical expertise in history taking and patient assessment is vital in ‘selecting’, which patients are suitable for a remote consultation verses a face-to-face consultation.
Some General Practitioner (GP) surgeries introduced patient email facilities such as ‘ASK MY GP’ (Digitalhealth.wales, 2020). Using this system, patients email their symptoms to their surgery and the GP either replies via email or telephone. Acute services and some GP surgeries introduced the combination of telephone, video consultations for example ‘Attend Anywhere’ (Digitalhealth.wales, 2020).
The principles of safeguarding and governance for remote consultations, assessment and prescribing is not dissimilar to conventional practice. For practitioners or service providers who are novice in their role or using remote consultation, the following practical considerations will inform their practise.
Preparing for a remote consultation
Some practitioners may conduct the consultation from non-traditional locations, such as their office or home especially if they are ‘shielding’ or ‘self-isolating’. It is important that their ‘office’ environment is appropriate and patient notes or data are not displayed. If working from home, safeguarding their own personal information is important and ensuring that the practitioners' relatives do not overhear the patients' consultation (Chua et al, 2020; GMC et al, 2019). Ideally, the use of a virtual private network system (VPN) issued from an NHS provider is recommended to ensure the online system is private and secure (Royal College of General Practitioners, 2020a).
In line with conventional in person consultations, it is essential that the practitioner has access to the patients most current medical records (General Pharmaceutical Council, 2019; Health and Care Professions Council, 2019, Nursing and Midwifery Council, 2019). Within Wales, most health care professionals (HCPs) have access to patients' electronic records which provide letters, GP medical notes and investigation results. When accessing the electronic records, the patients must provide verbal consent (GMC et al, 2019).
Conducting a remote consultation
For many patients, remote consultation would be a new experience, and some may feel apprehensive. It is advisable that a brief explanation of how the consultation will be conducted and the remedial plan if technical issues occur (Royal College of General Practitioners, 2020a).
For remote consultations, significant safeguarding and governance in regards the identity and confidentiality of both the patient and the practitioner is required. The patients' demographics must be confirmed at the start of the consultation and confirm their actual location (in case they are staying with relatives) should their condition deteriorate, and an emergency response crew is required (Royal College of General Practitioners, 2020a). Anecdotally, some services request photographic identification to confirm the identity of the patient to eliminate the risk of an online ‘imposter’. This is not standard practice for a conventional consultation as an ‘imposter’ could attend a traditional consultation too. Additional checks, known as ‘vouching’ (Royal College of General Practitioners, 2020a), could be applied by simply asking for the patients' allergy history or the name of a drug on their monthly prescription.
Introducing oneself in the same manner as a conventional consultation is essential. As is checking that the patient can hear clearly. This can be done by asking the patient a simple non-medical question such as ‘what is your address?’
Patient confidentiality in their home is essential. The patient is advised to check that the consultation cannot be overheard by other members of their household. If a relative or other person is present, their relationship should be confirmed by the patient, and it must be stated that their presence is consensual (GMC et al, 2019; Royal College of General Practitioners, 2020a). This should be documented in the patient medical records. If the consultation is recorded electronically, this must be transparent and consented to by all parties. Practitioners must have a justifiable reason to record a video consultation especially when undertaking a general or intimate examination (Royal College of General Practitioners, 2020a).
Communication skills
Regardless of the format of the consultation (face-to-face, telephone, video), a practitioner must have good communication skills to build a rapport with the patient. When using video consultations, they must be mindful of non-verbal communication as their face and eyes can be magnified on the patient's device screen. These can be addressed by careful positioning of the practitioner's camera (Chua et al, 2020).
Practitioners must make concerted efforts to ensure ‘human connectivity’, especially when using remote consultations (Chua et al, 2020). Many practitioners naturally have good communication skills, others need to master these skills. Remote consultations require greater clarity of expression; the appropriate use of open and closed questions is essential and will reduce the risk of ‘leading’ the patients answers. For example, instead of asking the patient if their ‘calf is red and swollen’, ask them to tell you what their calf looks like.
Clinical examination
A major challenge of remote consultations is the inability to perform examinations. This was an area of concern for patients (Powell et al, 2017) even before the pandemic's shift to remote consultations. Fortunately, this was addressed early in the pandemic by a flurry of publications on remote examination techniques such as David et al (2020) Ford and Hargroves et al (2020); Royal College of General Practitioners (2020a), Cortese et al (2020); Royal College of Psychiatrists (2020).
Each publication provides robust clinical detail and creativity combined with the ‘transferability’ of skills and competency from conventional in person examinations to remote examinations. For in person consultations, experienced practitioners use a clinical history combined with an intuitive ‘top to toe’ visual scan of the patient to construct a clinical picture and working diagnosis. This can be replicated in a remote video consultation by noting the patients' manner, appearance and clinically significant markers such as cyanosis or laboured breathing. Vital signs can be assessed remotely by requesting that the patient counts their own pulse or taps the approximate speed and rhythm. Anecdotally, the latter is standard practice in the assessment of new, unrecorded arrythmias (abnormal heart patterns). Also, some households have self-monitoring devices such as a smart device, mobile phone or watch, which can measure blood pressure or heart rate in addition to conventional blood pressure or temperature monitors. Whilst their validity cannot be quantified, they may offer some data for the practitioner.
Other clinical assessments can be carried out in different ways such as assessing respiration by instructing the patient to position their hand against their chest so the respiratory rate and chest movement can be reviewed. To assess functional capacity, patients can be asked to move from a sitting to standing position for 60 seconds; this can also be used to assess for postural hypotension or potential oxygen desaturation. The Remote Consultations Handbook (David et al, 2020) gives validated alternatives to face-to-face consultations.
Intimate examination
Practitioners are advised to be mindful of the need for intimate examinations. (David et al, 2020; Royal College of General Practitioners, 2020a). Intimate clinical examinations need to be dealt with sensitivity but cautiously. In line with conventional consultations and examinations, a chaperone should be used / offered and documented even if declined by the patient. Family members are not impartial, and their use as chaperone is not recommended. The Royal College of General Practitioners (2020b) provide very detailed guidance on dealing with remote intimate clinical assessments.
Remote prescribing
Before the pandemic, the Royal Colleges and many regulators collaborated to consider patient safety when consulting and prescribing remotely, and collectively produced the ‘high level principles for good practice in remote consultations and prescribing’ (GMC et al, 2019).
When prescribing remotely the same rigour and professional standards of prescribing in person must be observed. A detailed history, full medical and drug history including allergies, over the counter, herbal or recreational drugs, and medication adherence must be obtained (Royal Pharmaceutical Society, 2016). The clinician must be satisfied that remote prescribing is safe and appropriate for the presenting problem. If this standard cannot be achieved, careful clinical judgement must be applied, weighing up the context of the clinical problem, risks of virus transmission (during the pandemic), ability to apply and follow safety-netting plans and patient safety (GMC, 2020). If after due consideration, patient safety is compromised then remote prescribing cannot occur. A conventional in person consultation and prescribing must be offered or if not possible, the patient referred (signposted) to another service provider or health professional (GMC et al, 2019)
Safety-netting
Safety-netting outlines a clear plan for aftercare (follow-up) and instructions the patient should follow if their symptoms deteriorate or do not improve within a specified period. It should be used in conventional and remote consultations. David et al (2020) provide explicit and practical guidance as summarised in Figure 1.
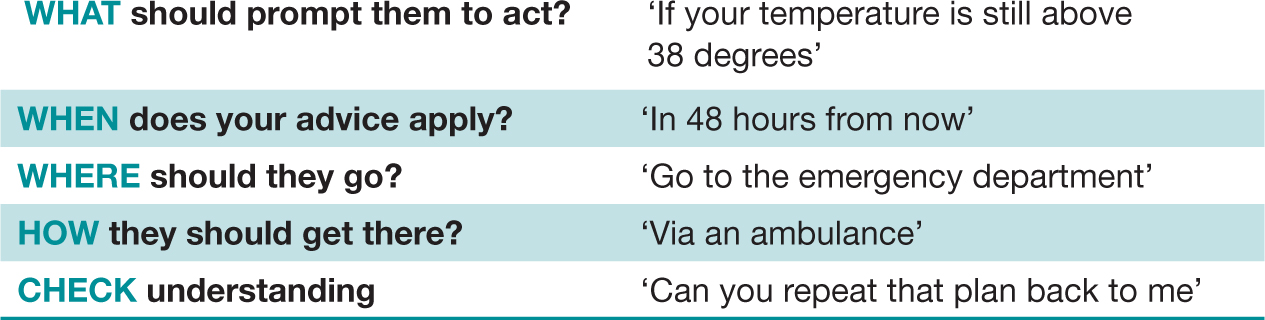 Figure 1. Safety-netting post remote consultation
Figure 1. Safety-netting post remote consultation
It is advisable to ask the patient to write the instructions down especially if they are elderly or there are any language or communication barriers. If unable to do this, they can ask a relative to write the instructions for them. Similarly, this and the follow-up plan must be documented in the patients medical records and communicated with other relevant health care professionals (GMC et al, 2019).
Documentation
It is essential that the consultation, its outcome: including prescribing, safety-netting and plan is clearly documented, along with its agreed format (telephone or video) (David et al, 2020; Royal College of General Practitioners, 2020). Any limitations of the consultations or examination must be documented. Similarly, the consultation and management plan, including prescribing and safety-netting must be communicated to all relevant care providers to ensure no omission or duplication of prescribing or care occurs.
Limitations of remote consultations
When considering the use of remote consultations, health care providers should be mindful that not all patients or healthcare professionals like or want remote consultations (Greenhalgh et al, 2018; Thiyagarajan et al, 2020). Some patient cohorts do not lend themselves well to remote consultations, such as patients with complex co-morbidity or those receiving palliative care (Greenhalgh et al, 2018; GMC, 2020).
Practitioners should be mindful, that remote clinical examinations often require significant patient or family interaction, for example following instructions to ‘take a pulse’ or ‘show the rash on your back to the camera’, this limits their universal adoption instead of conventional consultations (Greenhalgh et al, 2018).
Other barriers to the use of remote consultations and examinations include inequity in access to or ability to use computers proficiently, for example the elderly, homeless individuals, patients with learning needs, communication or language issues (Raven et al, 2013; Atherton et al, 2018). Also, vulnerable patients such as those experiencing abuse (privacy and confidentiality issues) or have mental capacity issues may render remote consultations unsuitable (Greenhalgh et al, 2018; GMC, 2020). Some healthcare professionals or sectors may know their patient cohort well enough to identify which patients fall within the above categories. But many will not have an existing relationship with the patient and have difficulty identifying which patients are suitable for remote consultations. Therefore, they must carefully assess whether remote consultation is in the best interest of each patient as an individual.
Governance
The COVID-19 pandemic forced healthcare professionals, managers and services to critically review their practice and facilitate innovation and creativity in the form of remote consultations and examinations. Prior to the introduction of remote consultations, employers and managers must take due diligence to ensure appropriate governance and safeguarding is in place. This will ensure quality of care, prescribing roles and responsibilities are not compromised (GMC et al, 2019).
Remote consultations offer creative alternatives to conventional practice; nevertheless, it is paramount that these are considered on an individual basis, within the context of the clinical situation and the risks associated with potential exposure or transmission of the virus. If limitations of the remote consultation are outweighed by the patients' clinical need, then a conventional in person consultation should be offered (David et al, 2020; Royal College of General Practitioners, 2020a; GMC et al, 2019). Of course, patient choice and their understanding of the risks / benefits of the clinical situation plays an important part too. However, it is vital that the patients' concerns are explicitly elicited and the pros and cons of the situation and the rationale for clinical decisions are communicated honestly and accurately to them.
For the practitioner, managing the above and determining a safe clinical outcome is based upon an amalgamation of complex decision processes which are the principles of advanced practice (National Leadership and Innovation Agency for Healthcare (NLIAH), 2010). Clinical knowledge, complex decision processes, governance and leadership are all key components of advanced practice (NLIAH, 2010; Anderson, 2018). These must be mastered and adhered to in order to work within a practitioner's scope of practice and competence. Understanding the importance of safe professional practice starts within education and training.
Virtual learning and assessment
Within the UK, the COVID-19 pandemic triggered a paradigm shift to remote consultations which accelerated the digitalisation of the National Health Service. Whilst the NHS was undergoing this digital change, education providers were simultaneously developing virtual platforms to serve learners needs. This required creativity, innovation and rigour to ensure continued compliance with professional regulatory standards.
Higher education, including NMP programmes, must be fit for purpose, research based and reflect clinical practice. It should also lead and innovate practice. The COVID-19 pandemic dictated that academics work differently (via a non-face-to-face format) to provide education. This necessitated a departure from traditional teaching methods to a more blended learning approach.
Blended learning
The term ‘blended learning’ has many different meanings, but in this context, it is used to describe a blend of online teaching, self-directed learning with minimal face-to-face teaching. Although the NMP academic team had previously used technology to support teaching and learning, they had no experience or awareness of the principles needed for meaningful online learning experiences (Rapanta et al, 2020). This necessitated new learning to use additional resources for teaching such as ‘Zoom’ and ‘Microsoft Teams’ communication systems. This would require a new approach to the organisation and support for learning (Bates and Poole, 2003).
Despite the need for change, the quality of learning could not be compromised as non-medical prescribing is a professional qualification regulated by the General Pharmaceutical Council, Health and Care Professions Council and the Nursing and Midwifery Council. All of the regulators expect rigorous standards to be upheld to ensure the principles of safe prescribing are maintained even during the pandemic. Mindful of this, the learning outcomes for each professional regulator were revisited to ensure that the learning journey and assessments were aligned (Bates, 2019). In addition, the NMP academic team acknowledged the work Munoz and Mackay (2019) and the challenges of assuring quality and validity of the assessment strategy when being conducted online. Each regulator was informed of the changes, which were subsequently agreed, as they did not impact on the scholastic learning outcomes.
Transition to virtual learning
At the height of the first wave of the pandemic, the existing NMP cohort had completed most of their assessments, but their clinical consultation assessment was outstanding. Following discussions with learners and the university, it was agreed that the assessment (conducting a patient consultation, diagnosis, prescribing, safety-netting / health advise and discussion about a patient scenario) would be undertaken via individual ‘Zoom’ meetings. Surprisingly, this cohort of learners reported (anecdotally) feeling less ‘stressed’ or anxious compared to ‘normal’ in person assessments. Other reported benefits were not needing to travel to the university for their assessment. Negatives were related to technical issues such as temperamental internet connection and learners' unfamiliarity of the new assessment format for example how could they demonstrate examining the chest via a Zoom meeting format.
The next cohort were aware that the NMP education programme would be delivered via a blended learning format. Both the NMP academic team and learners were mindful of the unprecedented situation afforded by the pandemic and there was a cohesive ‘team spirit’ and tolerance in trialling new teaching methods and opportunities. Despite this, challenges were anticipated, especially as coincidentally, the University had purchased a new virtual learning platform (CANVAS), which the NMP academic team were unfamiliar with.
There were numerous new issues for teachers and learners. From the academic perspective these included new technology, new learning platform (CANVAS) and changes in teaching methods and assessments. In regards the learners, most of them had changed their ways of working in clinical practice and had adopted remote working systems (remote consultations). Due to the pressures of the pandemic, many learners were having to work clinically during normal University hours. Therefore, greater flexibility of the NMP academic team was key, for example some Zoom teaching sessions were offered outside traditional university hours. Integrating these changes into the NMP course was a mammoth task for both the NMP academic team and the learners alike. Listening to the learners concerns and maintaining channels of active communication was paramount for success.
Learner survey and feedback
The NMP academic team were mindful of the stresses that this new untested way of teaching and learning would bring for the learners. Many learners were already under considerable strain in their workplace, and both factors could impact upon their ability to learn (Bates, 2019). For this reason, a variety of teaching modes were chosen to deliver learning initially. After approximately 6 weeks of teaching, a voluntary online survey was undertaken to assess the learners perceived confidence in learning through the virtual format. The questions used a five-point Likert scale format which aimed to elicit the learners concerns and identify whether there was a preference for a specific learning style.
The NMP acknowledge a major limitation of the survey was that it was not anonymous. Despite this, the response rate was good with a 62% response rate (n=17). Table 1 illustrates: prior to starting the course, the learners were apprehensive about the transition to virtual learning, but reassuringly there was greater positivity 6 weeks into the course (Table 2).
 Table 1. NMP learners' feelings about change to virtual learning
Table 1. NMP learners' feelings about change to virtual learning 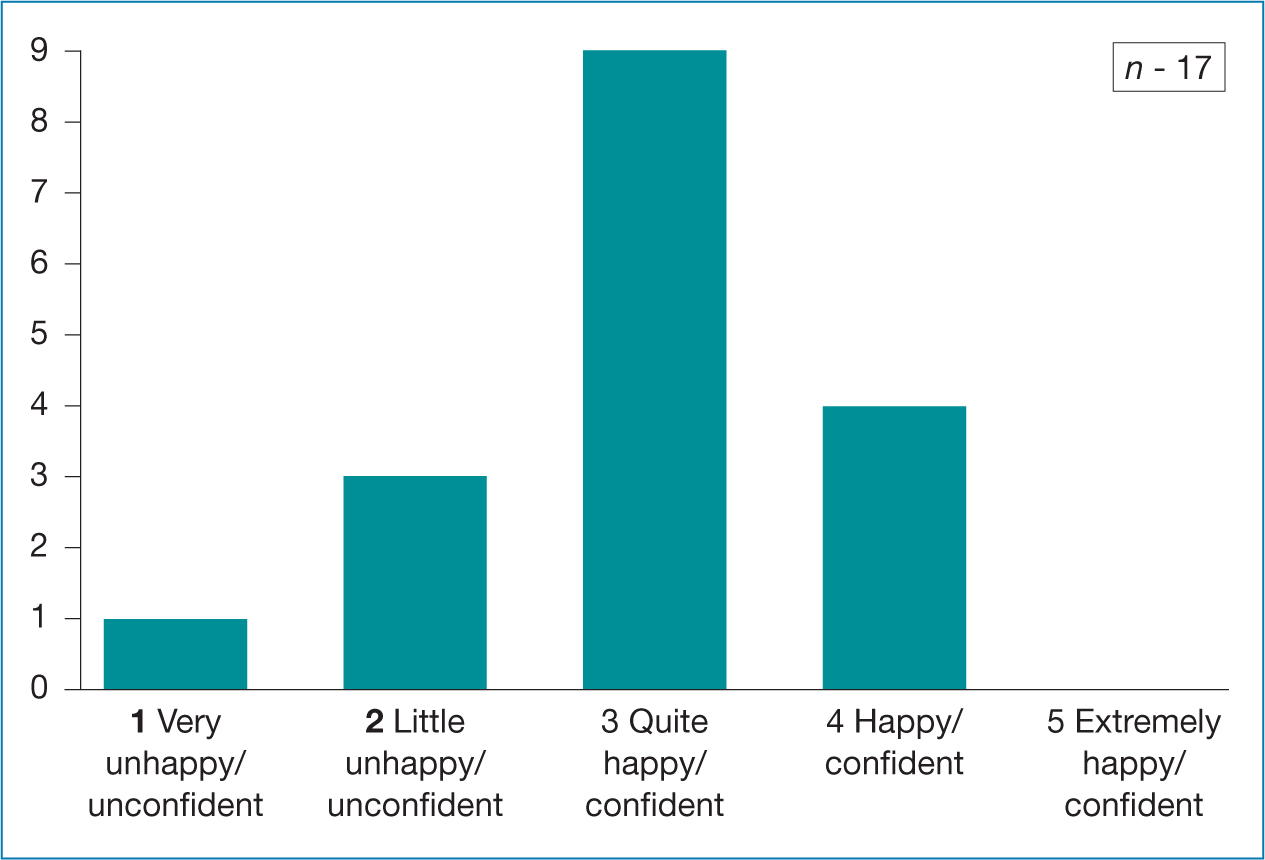 Table 2. NMP learners - How happy and confident are you with blended learning?
Table 2. NMP learners - How happy and confident are you with blended learning?
Regarding which mode of teaching was most suitable to their learning needs; Tables 3-7 show there was a broad range of the responses with no consensus apart from a preference towards the live ‘Zoom’ catch – up and discussion sessions. The comments section identified that some learners were frustrated by the technical issues associated with the new virtual learning platform resulting in numerous emails being sent to them with attachments of learning materials (PowerPoints and notes).
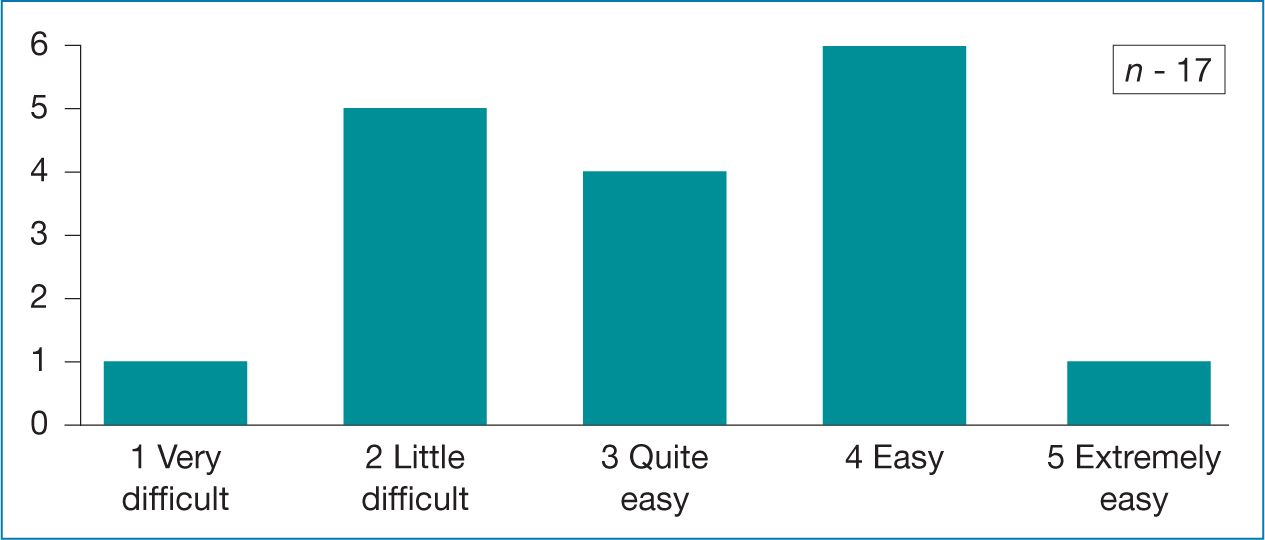 Table 3. NMP learners views on silent PowerPoint presentations
Table 3. NMP learners views on silent PowerPoint presentations 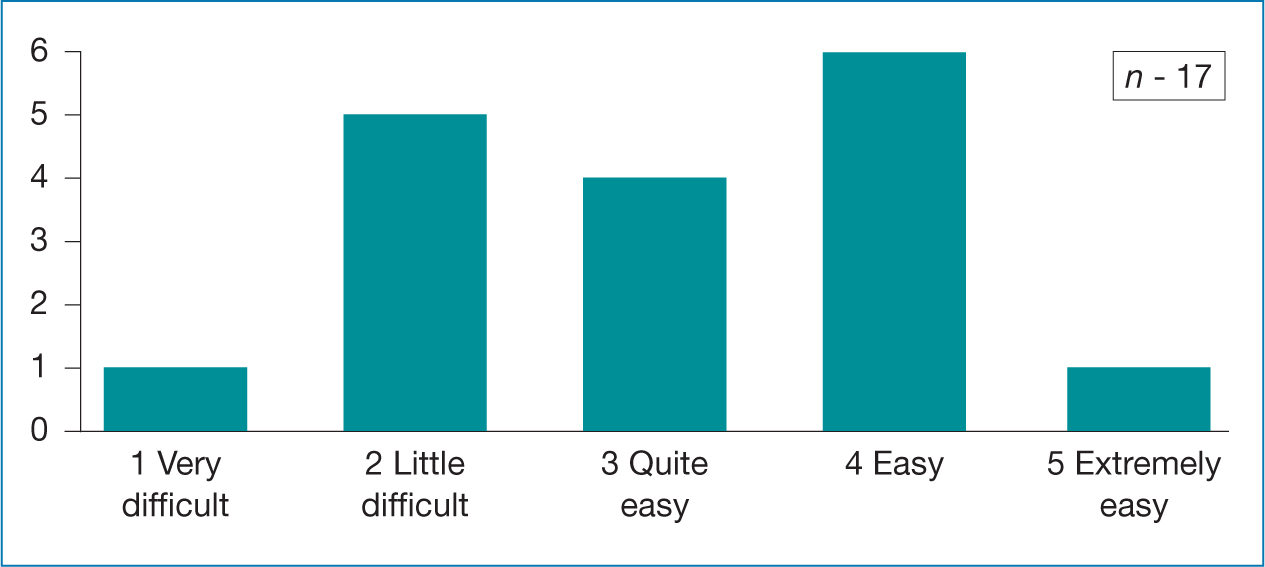 Table 4. NMP learners views on PowerPoint with audio presentations
Table 4. NMP learners views on PowerPoint with audio presentations 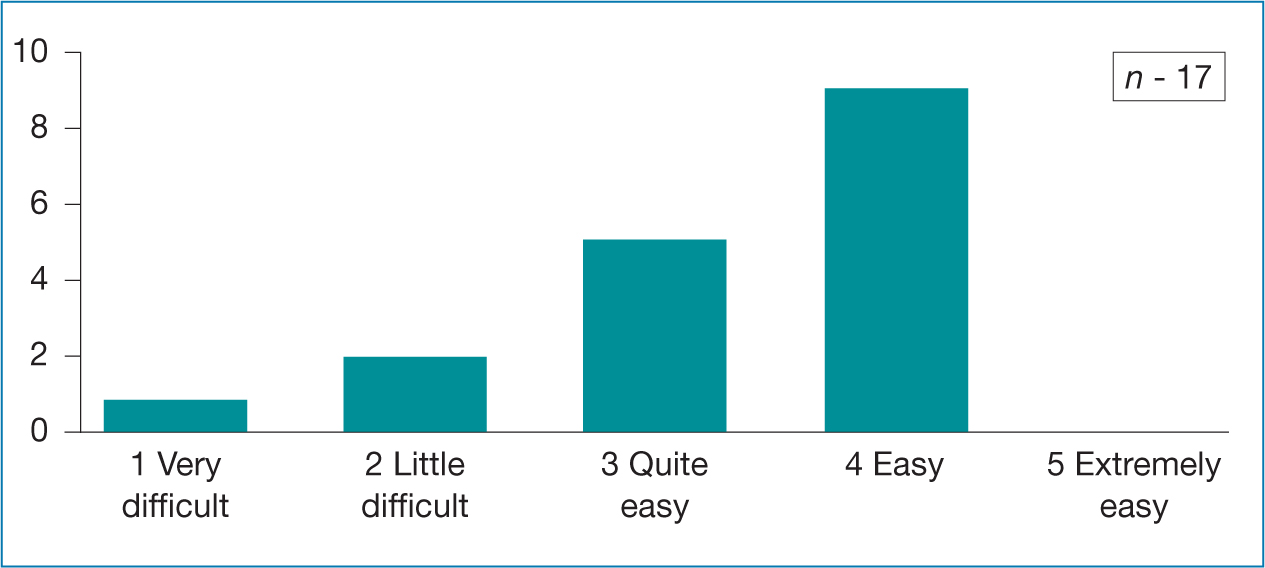 Table 5. NMP learners views clinical videos
Table 5. NMP learners views clinical videos 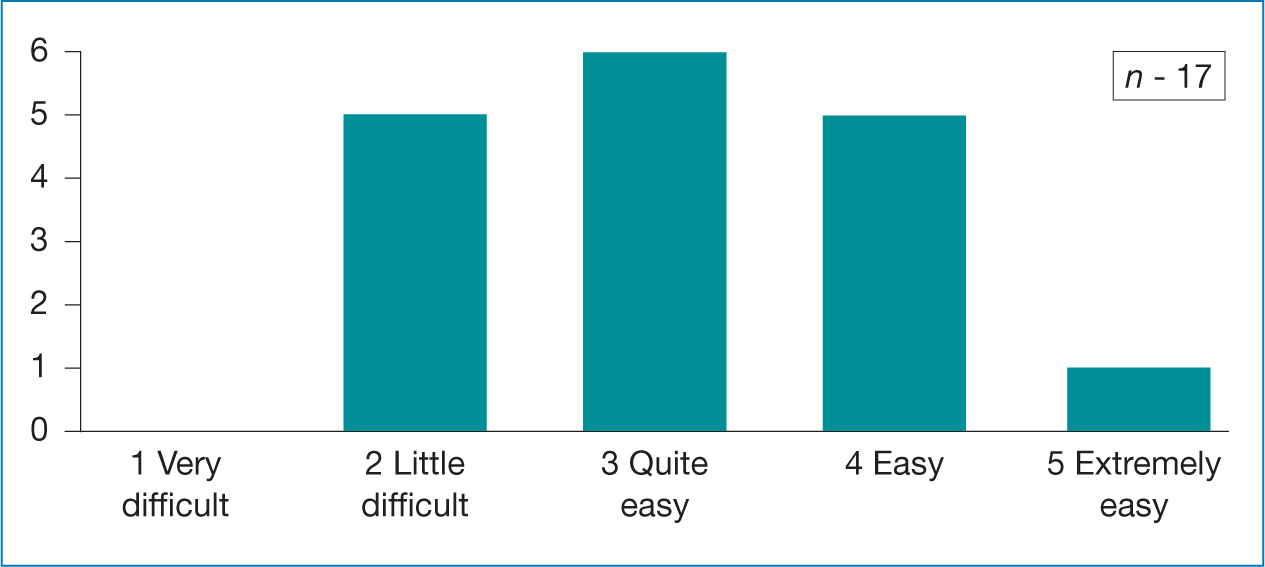 Table 6. NMP learners views Xerte-silent reading
Table 6. NMP learners views Xerte-silent reading 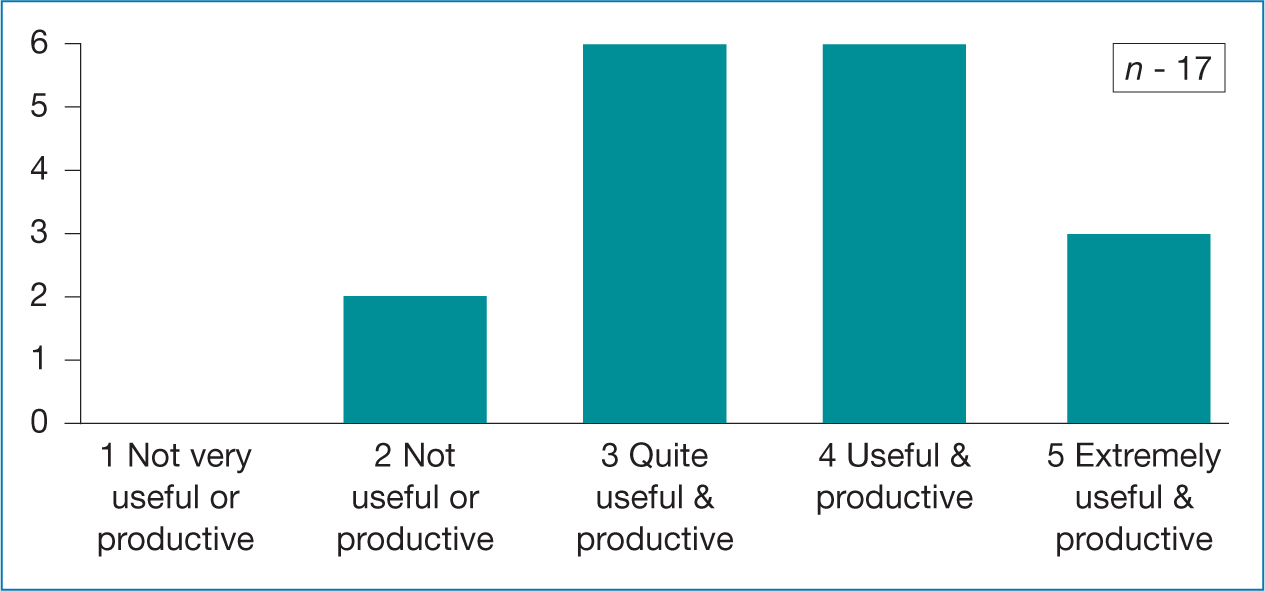 Table 7. NMP Live ‘Zoom’ catch – up / discussions
Table 7. NMP Live ‘Zoom’ catch – up / discussions
Later in the programme, the learners participated in the University's ‘Listening Forum’. This forum is facilitated by the ‘Student Experience Team’, where learners anonymously raised points which are subsequently addressed by the NMP academic team. The forum identified that they felt more isolated compared to traditional in person teaching, and suggested lunchtime Zoom meetings to help build relationships and network with colleagues. This isolation impacted on their confidence too as they felt their queries were too trivial to warrant a one-to-one Zoom meeting with the NMP academic team.
Learner personal experiences
Two of the NMP learners kindly shared their personal experiences for this article. Five common themes were identified, technology issues, camaraderie, isolation, virtual learning and remote consultations.
They described concerns about the move to remote / virtual learning. The new virtual platform (CANVAS) was a significant challenge and source of frustration which was worsened by poor broadband connection or non-compatibility of NHS software.
They appreciated the NMP academic teams' efforts in rectifying technical problems and how they were actively encouraged to feedback issues or suggestions for improvements to their learning experience.
They felt that the technical challenges created ‘a sense of camaraderie’ amongst the learners and lecturers, which grew as the course progressed through the ‘shared experience’ of using alternative methods of learning.
Remote learning eliminated the need to travel to university, allowing more time to be diverted to study time. This permitted them to study at their own pace and ‘dip in’ and prepare for the virtual teaching sessions at their convenience. However, ‘computer fatigue’ was an issue. This reflects concerns identified previously by Bates (2019).
They valued the flexible support (via phone, email or zoom meetings) from the academic team as this helped to alleviate ‘feelings of isolation’. The loss of peer support from the classroom and the need to study alone was an area of concern and exacerbated the feelings of isolation.
The introduction of remote consultations and remote learning had a huge impact on both their learning and ‘real-life’ clinical practice.
They felt the move to virtual learning placed greater emphasis upon the teaching of clinical skills in their practice learning environment. They valued the mock clinical assessments and peer revision zoom groups. The latter unexpectedly helped build rapport and relationships within the group.
The need to use advanced communication skills, clinical reasoning, analytical thinking whilst simultaneously conduct a virtual assessment was challenging for the learners but they acknowledged the importance of mastering these skills in order to be safe, competent prescribers. They felt the adoption of remote consultations had positively changed their practice and equipped them well for independent prescribing status.
Overall, after reviewing the outcome of the questionnaire, the ‘Listen forum’ and personal learner experiences, the NMP academic team concluded that despite the challenges, the learners tolerated the transition to virtual learning well and demonstrated great resilience.
Conclusion
During the pandemic there has been a paradigm shift to remote patient consultations and prescribing. A precedence has been set and remote consultations will become standard practice. However, in person consultations will always be needed and cannot be universally replaced. The decision to use remote or in person consultations must be based upon clinical need, risk stratification and patient choice. Regardless of the format of the consultation (telephone, video or face-to-face), non-medical prescribers must always have adequate clinical detail, safety netting processes and documentation in order to prescribe safely (General Pharmaceutical Council, 2019; Health and Care Professions Council, 2019; Nursing and Midwifery Council, 2019; Royal College of General Practitioners, 2020a) and adhere to the high level principles of remote consultation and prescribing (GMC et al, 2019).
The COVID-19 pandemic necessitated a fusion of proactive, purposeful collaborative working between academics and healthcare. This has always been present but now there is a new alacrity. For the NMP learners studying at Swansea University, it undoubtedly felt like a ‘rocky road’ and challenging journey but they are commended for their professionalism and determination to embrace the transitory changes. From an academic perspective, the NMP academic team also positively embraced the need for rapid change. They used creativity to innovate both clinical practice and teaching whilst adhering to the regulations and standards of the three professional bodies.
The shift from the classroom to virtual has many similarities to consulting remotely, there are principles and standards that must be maintained, but with good communication and flexibility from all parties, these new ways of working can bring benefit for everyone.
The academic team maintained the fundamental goal of ensuring its NMP learners are confident, competent and safe prescribers. The learner's goals are to achieve the best outcomes for patients whilst minimising harm.


