Since 2006, physiotherapists have been able to train as supplementary prescribers, following the ground-breaking work of Crown (Department of Health [DoH]1989;1999); and since 2013, they have been able to train as independent prescribers (IPs) (DoH, 2013). Prescribing has been claimed as an essential component in expanding physiotherapists' scope of practice (Morris and Grimmer, 2014). However, at the time of conducting this study, statistics indicated that out of 55 140 registered physiotherapists in the UK (Health and Care Professions Council [HCPC], 2018a) only 1.46% (n=807) were supplementary prescribers and 1.24% (n=681) were IPs; meaning that under 2% of the available population have undertaken training to become a prescriber, compared to 15% of pharmacists and 6% of nurses, as stated by the HCPC (2018b) as well as in email correspondence with the General Pharmaceutical Council (received 13 August 2019) and Wickham (received 29 April 2019).
Non-medical prescribing (NMP) (ie prescribing by healthcare professionals other than doctors and dentists) in general is well developed and there is evidence that it is clinically safe, cost-effective and acceptable to patients (Cope et al, 2016). Cope et al (2016) echo work by Courtenay et al (2011) who commented on how patients valued the combination of the prescribing and caring role of nurse non-medical prescribers. Since the introduction of NMP, the number of non-medical prescribers has grown to 90 000 (Carey et al, 2020). While the administration of medicines in the form of injection therapy by physiotherapists has been recognised as producing a more consistent and transferable workforce (Atkins, 2003), there is a lack of published evidence to date with regards to the effectiveness of prescribing by physiotherapists (Robertson et al, 2016), which is likely to continue while numbers remain small. This continues to be the case, as highlighted by Stenner et al (2018) and confirmed by Carey et al (2020) leading to a paucity in published research on physiotherapist prescribing. Understanding the possible barriers that physiotherapists perceive as preventing them from becoming prescribers, as well as their general attitudes towards medicines, could help identify potential support for physiotherapists in future, enabling more to utilise their right to prescribe. This pilot study gives insight into key areas to explore when assessing physiotherapists' readiness and willingness to take on prescribing as part of their practice and can inform a larger study in future.
This pilot study aimed to explore the attitudes of qualified physiotherapists working in a variety of health settings towards prescribing and medicines as part of their practice, identify barriers to implementation of prescribing and determine their training and information needs regarding medicines management.
Study design
The study comprised two phases. In phase one, an expert group devised a questionnaire which was tested with a small subset of physiotherapists utilising cognitive interviewing for content validity. Feedback received from these physiotherapists was used to make adaptations to the final questionnaire before phase two, which saw the distribution of the questionnaire to a wider professional population of physiotherapists via social media and online networks.
Ethical approval was obtained from the Medway School of Pharmacy (Universities of Kent and Greenwich) Research Ethics Committee (REC).
Sample size and recruitment
A pragmatic approach was taken to select an appropriate number of phase one participants. Twelve individuals were identified through local physiotherapy networks and invited to take part to ultimately obtain six participants. Participants were recruited using the networks of three gatekeepers – a pharmacist independent prescriber who works with physiotherapists, a physiotherapist independent prescriber and a pharmacist specialising in medicines management advice to elite sporting teams.
Given the pilot nature of the study, a sample size of 50 questionnaire completions for phase two was deemed appropriate.
Participants were recruited in the same manner as for phase one, utilising the networks of the three gatekeepers for the project. A snowball sampling approach was taken, where participants were recruited via websites such as LinkedIn, Twitter, Facebook and any other professional (non-NHS) groups of the gatekeepers. The gatekeepers shared the questionnaire link throughout these networks, recruiting participants, who further shared the questionnaire link.
Inclusion criteria
Participants for the cognitive interviews and the online questionnaire needed to be currently working (or had been working in the last 2 years) in the UK in NHS or private practice as a physiotherapist, and had been on the HCPC (the regulatory body for physiotherapists) register for a minimum of six months).
Instrumentation
An expert group was convened consisting of: a physiotherapist independent prescriber, a pharmacist specialising in medicines management advice to elite sporting teams, a Clinical Commissioning Group (CCG) medicines management lead (and pharmacist IP) and a nurse prescriber with experience in general practice. The group attended a workshop facilitated by the lead researcher, which led to the first draft of the questionnaire using the consensus opinions of the panel, and a literature search carried out by the physiotherapist independent prescriber. The questionnaire was created using the Qualtrics platform (Qualtrics, 2017) and consisted of sections including;
- Demographics
- Attitudes to medicines
- Attitudes to prescribing
- Impact of work environment
- Preparatory training requirements, containing 43 questions of varying formats.
The number of questions differed depending on whether the participants were prescribers or not. Subsequently, the questionnaire was made available online via a link to the Qualtrics platform for use in phase one.
Revision to questionnaire using cognitive interviews - phase one
Cognitive interviews with six physiotherapists utilised think-aloud and verbal probing approaches to review phase one questionnaire content and meaning. Comments collected during cognitive interviews were assessed by the expert group with subsequent alterations made to the questionnaire for phase two of the pilot study. The expert group collated the comments made by the participants in the cognitive interviews and made changes to the questionnaire in support of clarity and meaning. The process of content validation was carried out once, leading to the second iteration of the questionnaire being the final version.
Procedures – phase two
The revised questionnaire was sent out via email through the networks as detailed above. Reminders were sent through the same online networks 7 days later with the questionnaire open for 2 weeks.
All online questionnaires returned through Qualtrics© were anonymous.
Data analysis
Data were principally quantitative with some qualitative free-text sections. The Statistical Package for the Social Sciences (SPSS) (IBM, v25) and Microsoft Excel were used to manage the data.
Statistical significance was set at the value of 0.05 and statistical tests were used to examine the significance of any differences or associations in the data. Data were predominantly categorical, however, questions which were assigned to a Likert scale format were treated as ordinal data, as each response was allocated a value/score. This meant that increased agreement had a lower value/score than increased disagreement. Thus, parametric statistical tests such as independent t-tests were used. Nonparametric statistical tests such as Mann Whitney U and the Chi-Square test of association were also used – the latter on categorical data. Qualitative data were analysed for patterns and common themes. Qualitative data in the form of free-text answers to questions were collated and subjected to thematic analysis (Braun and Clarke, 2006) in order to identify common themes. Responses made in text form were reviewed for common themes prevalent within the responses., providing insight into beliefs and opinions shared by physiotherapists. Qualitative data was inputted using Microsoft Excel whereas Quantitative data utilised SPSS.
Findings: questionnaire phase two
Demographics
There were 51 respondents to the questionnaire. Table 1 shows the demographic details of the participants.
Table 1. Demographic data
| Gender | ||
|---|---|---|
| Frequency | Percentage | |
| Male | 20 | 40 |
| Female | 30 | 60 |
| Prefer not to say | 1 | 2 |
| Age | ||
| 25 years or less | 1 | 2 |
| 26-35 years | 14 | 28 |
| 36-45 years | 19 | 38 |
| 46-55 years | 15 | 30 |
| 56-65 years | 1 | 2 |
| Age not provided | 1 | 2 |
| Mean age (years) | 40 | |
| Median age (years) | 38 | |
| Qualified in the UK | ||
| Yes | 46 | 92 |
| No | 5 | 10 |
| Prescriber status | ||
| Supplementary/Independent prescriber (dually qualified) | 19 | 38 |
| Not a prescriber | 32 | 64 |
| Number of years practising | ||
| 0-5 years | 4 | 8 |
| 6-10 years | 4 | 8 |
| 11-15 years | 16 | 32 |
| 16-20 years | 10 | 20 |
| 21 years and above | 17 | 34 |
| Work for the NHS | ||
| Yes | 33 | 66 |
| No | 18 | 36 |
| Main work setting | ||
| Primary care | 15 | 30 |
| Secondary care | 17 | 34 |
| Private (including AQP)* | 19 | 38 |
| Area of practice | ||
| Neurology | 2 | 4 |
| Respiratory | 2 | 4 |
| Palliative care | 1 | 2 |
| Frailty | 3 | 6 |
| Adult MSK** | 23 | 46 |
| Other | 8 | 16 |
| Sports physiotherapy | 12 | 24 |
| Other | 8 | 16 |
MSK - Musculoskeletal
Attitudes to medicines
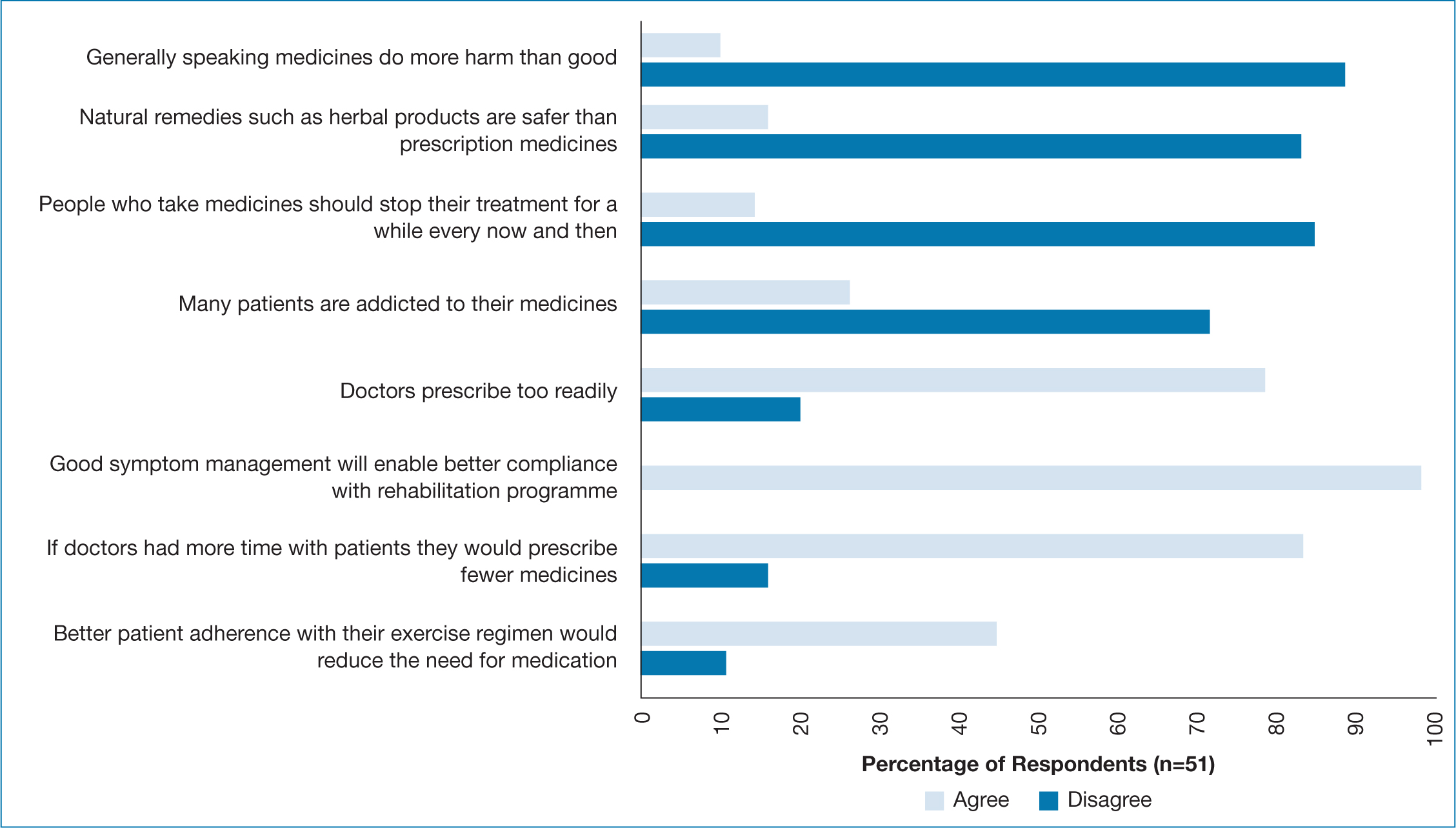
Attitudes and beliefs towards medicines were assessed in section two of the questionnaire, using a Likert-scale format. The responses are shown in Figure 1. The majority of respondents (90%, n=46) disagreed with the statement that medicines do more harm than good. There was also disagreement with the statement that natural remedies such as herbal products are safer than prescription medicines (84%, n=43). Most respondents believed doctors prescribe too readily (80%, n=41), and if they had more time with patients, they would prescribe fewer medicines (84%, n=43). Prescribing physiotherapists showed no greater likelihood to prescribe medication for low back pain than their non-prescribing colleagues, whilst prescribers were less likely to advise rest than their non-prescribers (prescribers 5% n=18, non-prescribers 33% n=30).
Attitudes to prescribing
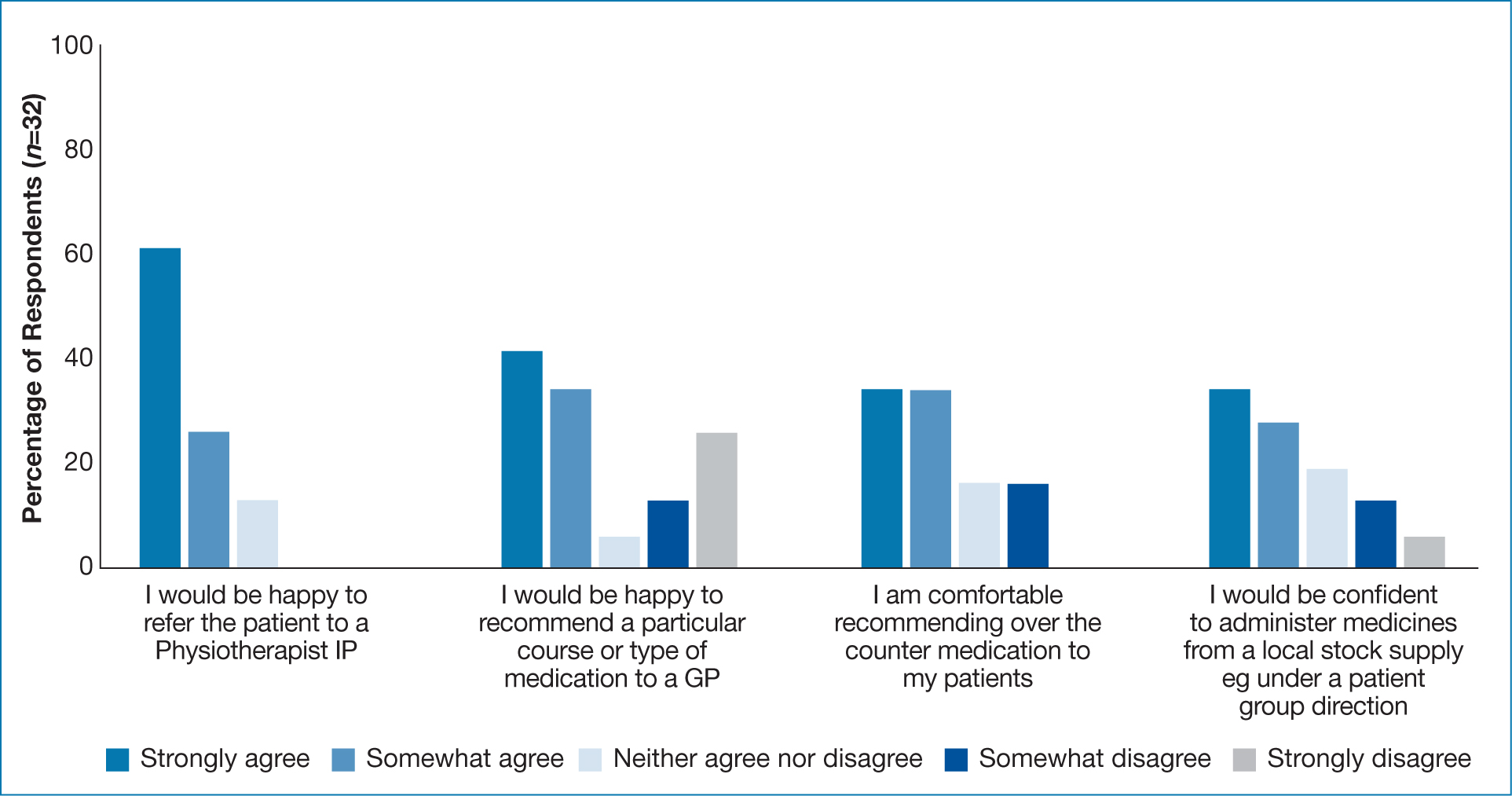
In section three, physiotherapists who identified themselves as not prescribers were asked to indicate their level of agreement or disagreement with a set of statements relating to their attitudes towards prescribing (Figure 2). Of the 32 non-prescribers, 61.3% (n=19) were happy to refer patients to a physiotherapist IP. Only 13 (40.6%) were happy to recommend medication for a GP to prescribe. On questioning 34.4% (n=11) would recommend an over the counter medicine to a patient and the same number would happily administer medicines (34.4%, n=11).
Impact of work environment
Questions regarding the impact of the working environment were asked of all the respondents. Here ‘n’ refers to the number of participants and not to any specific grouping of prescribing or non-prescribing. Data showed that 46% (n=23) indicated their work environment supported prescribing by healthcare professionals other than doctors, whilst 40% (n=20) indicated they received ‘no support’.
Participants with workplace support were found to be significantly more likely to be working in the NHS than in private practice (p= 0.001; t=-3.537).
Nearly half (48%; n=24) of the 51 respondents specified that there were no other non-medical prescribers in their organisation. When asked if their organisation understood the role of the NMP, 32% (n=16) of all respondents stated yes.
The data was further examined to see whether there was a significant difference between physios working in different settings with the majority of respondents who agreed that their work environment supported NMP reporting that they worked within secondary care (48 %, n=11).
Preparatory training requirements
The majority of respondents indicated that basic pharmacology (85%, n=39) and legal aspects (81%, n=38) were knowledge physiotherapists require prior to prescribing.
Qualitative assessment
Free text answers provided by participants were divided into answers provided to questions aimed at both prescribers and non-prescribers or prescribers and non-prescribers exclusively. The following themes were generated: lack of pharmacology knowledge, responsibility and frustration.
When asked about training needs, participants (prescribers and non-prescribers) cited ‘depth of knowledge of pharmacology’ and ‘greater ability to explain the actions and benefits of medicines to patients’ as areas of need. Suggesting a lack of pharmacology knowledge as a theme. Training as a prescriber appears to be perceived by physiotherapists as enabling thinking about pharmacology and increasing the likelihood to consider medication change as part of the consultation with prescribers stating that they are ‘more open to the role of medication as an adjunct to therapy. Better able to provide a stepwise approach to treatment modalities’.
Meanwhile, some responses showed an increased hesitancy in prescribing for patients for example: ‘More cautious of medication usage, due to increased awareness of interactions, side effects.’
Prescribing physiotherapists (n=19) were asked to explain whether their attitudes towards medicine use had changed since they undertook their training. A Common theme which arose was increased knowledge about pharmacology. A theme of responsibility arose with participants sharing opinions such as ‘Now more aware of the clinical reasoning for not prescribing than before my training’. ‘Empathy with doctors who prescribe in polypharmacy situations’ was also expressed. The personal and professional benefits that prescribers said medication prescribing brought them included increased job satisfaction and autonomy, better/more holistic patient care, cost and time savings and professional development.
Existing prescribers (n=19) were asked to indicate the type of difficulties they had experienced or anticipated experiencing when using their prescribing qualification. Recurring themes from the free-text responses were personal difficulties such as lack of confidence as a new prescriber. Organisational difficulties included a lack of funding to prescribe and a lack of peer support and understanding from colleagues. Although lack of support was reported by only one participant who stated a ‘Lack of peer support, difficulty becoming registered with an employer, lack of appropriate environment or funding in which to prescribe.’ These linked with professional difficulties cited by physiotherapists predominantly consisted of legal restrictions. With a common theme of frustration concerning the current limitation of prescribing controlled drugs to a list of seven drugs.
Those participants who were not prescribers (n=32) were asked if they had considered undertaking prescribing training. Of these, 13 (41%) had considered it, 11 (34%) had not and four (13%) were already undertaking training. Two respondents stated that they ‘did not want to prescribe’, two stated their job role was not conducive, another said there were ‘barriers in current role’ and one stated they were ‘fearful of prescribing’. The comments provided by physiotherapists in this section suggested a number of different unrelated reasons rather than any underlying theme but suggest a disconnect with prescribing within the profession, which reflects findings by Noblet et al (2019) in their study looking at the perceptions of physiotherapists regarding the implementation of prescribing in Australia.
Discussion
The pilot study explored the attitudes of qualified physiotherapists working in a variety of healthcare settings towards prescribing medicines as part of their practice. We identified barriers to implementation of prescribing and requirements for physiotherapist training and information needs regarding medicines management.
The demographic data collected in the pilot revealed a male to female ratio of almost 2:3, slightly higher than that suggested by the national demographics (HCPC, 2018c). The majority of respondents were highly qualified and reported experience in excess of 10 years, which is corroborated by a large study evaluation of physiotherapy and podiatric prescribing (Carey et al, 2017).
While the majority of respondents agreed with commonly agreed precepts upheld by evidence-based medicine regarding the overall beneficence of medicines, up to 1:6 respondents reported beliefs that natural remedies were safer than prescription medicines. This suggests that a substantial number of physiotherapists could hold beliefs that natural remedies are safer than prescription medicines, a belief that could have a significant impact on discussions with patients.
Prescribing physiotherapists were no more likely to advocate prescribing medication for low back pain than their non-prescribing colleagues and reported an enhanced awareness of the responsibility associated with prescribing, especially in areas of polypharmacy and medication burden for elderly and frail patients. Of considerable interest is the relatively high percentage (approximately 40%) of physiotherapists non-prescribers who suggested that they may have potential concerns regarding referring patients to a prescribing colleague. Further work to investigate why these attitudes are held could potentially help to educate physiotherapists on the role and extent of NMP in physiotherapy management. This finding suggests potential discordance within the profession relating to the use of NMP that is revealed in work by Noblet et al (2019) where almost one in eight Australian physiotherapists commented that they did not feel that prescribing was or should be within the remit of physiotherapy. Interprofessional issues such as this are also to be noted by Emary and Stuber (2014) who studied chiropractors' views on prescribing. Similar beliefs were expressed with a significant number of those surveyed arguing against the development of full prescribing rights as it was believed to impact on their role identity. This may be a topic for future research.
In this current pilot study, the majority of respondents indicated that basic pharmacology and legal aspects were two areas of knowledge considered important for physiotherapists to become cognisant of prior to undertaking prescribing training. These concerns echo that of Cabilan et al (2016) who argued that knowledge of medication and how medication works is an area of weakness among nurses who undertake prescribing programmes
It was both surprising and disappointing to see the number of respondents reporting a lack of workplace support. This is of real concern considering the development in the profession of the first contact practitioner (FCP) role in primary care, where patients can access a FCP who may be a nurse, pharmacist, physiotherapist or paramedic at their GP surgery without having to see a doctor first. Whilst it is comforting that support within the NHS was reported as more likely with the growth and development of provider services, especially in MSK and FCP services, there is a clear need for the profession to provide suitable support for newly qualified prescribers. Nearly half of those who completed the questionnaire had no other prescribing colleagues in their organisation with a minority reporting that the organisation understood non-medical prescribing. While this could reflect the low numbers of prescribers within physiotherapy, this is again a cause for concern reflecting a worrying level of potential ignorance with regards to the role of NMP within organisations even after the prolonged length of time since the inception of NMP. It is not surprising that organisations the participant perceived as not understanding the role of NMP and its benefits were stated to have lower numbers of prescribing physiotherapists as employees. The ongoing level of lack of awareness is also reported by Graham-Clarke et al (2018) who state in their systematic review of NMP that managerial awareness can be both an enabler and a barrier to the development of NMP. Poor managerial support is equated with a barrier to development and high levels of confidence and support were correlated with increased use of non-medical prescribing. Barriers to prescribing have previously been cited by Courtenay et al (2018) who highlighted key themes that enable the development of barriers to prescribing including lack of an organisational strategic vision for non-medical prescribing and lack of managerial support.
Conclusions
There continue to appear to be barriers to physiotherapists embracing prescribing as a profession and appears to be an approach currently undertaken by physiotherapists who have a significant time post qualification in clinical practice, despite benefits reported by physiotherapists who have undertaken prescribing. There remain frustrations at the issue surrounding prescribing of controlled drugs and the support of prescribers in the workplace remains a critical need.
As a pilot study the questionnaire was only open for a short period of time, which limited numbers. It was not possible to calculate a response rate as it was not possible to know how many people viewed the questionnaire. Since respondents were recruited through the gatekeepers, limited by the size and nature of their professional contacts, the sample size for this study was lower than that of studies which adopted a similar questionnaire-based approach (Lansbury and Sullivan, 1998; Grimmer et al, 2002) but is appropriate for a pilot study.
The literature indicates that financial factors are significant facilitators or barriers to NMP, this includes funding for the time and education that prescribing entails, as well as financial support for the completion of the course and subsequent CPD (Noblet et al, 2017). The lack of funding to utilise their prescribing skills was defined as a difficulty by respondents within this study, however, the final questionnaire did not specifically ask about financial factors.


