A – Absorption
It is commonly stated that children are not just small adults; yet, most paediatric medication doses are still calculated from studies in adults (O'Hara, 2016). A knowledge of physiological differences between children and adults is imperative to have a thorough understanding in differences in pharmacokinetics.
Unless administered intravenously, drugs need to cross semipermeable cell membranes before they finally reach the systemic circulation. There are many other ways in which drugs are administered by extravascular routes, such as via the gastrointestinal (GI) tract, topical or transdermal, and through the lungs being the most common routes (van den Anker et al, 2018). Most drugs in children are administered orally. The taste of medications is an important factor (see ‘T’ later in this series), as children will naturally reject bitter or foul-tasting medications. However, once successfully taken, drugs will enter the stomach and gastric pH needs to be considered (Figure 1).
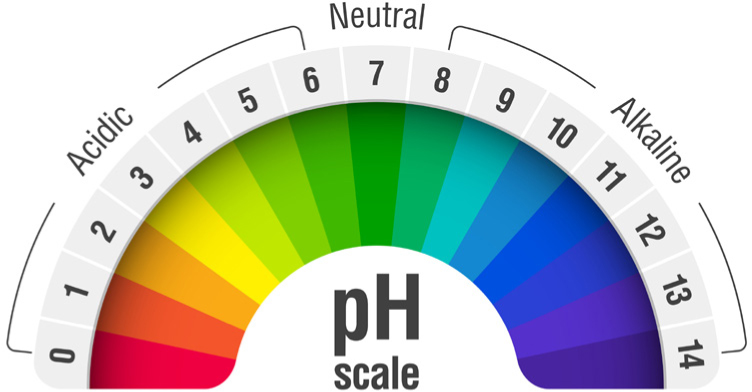
Gastric pH is neutral at birth, but falls to very acidic levels of 1–3 up to 48 hours after birth. By the time the infant is a week old, the pH will return to neutral, and finally will reach adult values around 2 years of age (Lu and Rosenbaum, 2014). This higher pH will have an effect on acid labile drugs, and may account for higher bioavailability (the extent to which the drug becomes ‘available’ to its intended destination) of beta-lactam antibiotics, such as penicillin. Conversely, weak acid drugs, such as phenytoin or phenobarbitone, will have a reduced bioavailability.
Gastric emptying time is also a factor: it can take up to 8 hours in neonates and young children, which can result in an increased absorption of some drugs, due to reduced motility. Other GI differences include biliary function, resulting in a reduced ability to make lipophilic drugs more soluble (Sage et al, 2014), and a reduced bowel length, resulting in a smaller absorptive surface.
Rectal administration is an option if oral administration is not possible. The rectum has a rich blood supply, but absorption time in children is variable (Skinner, 2008), and young children have more frequent large muscle contractions so expulsion of the suppository is a potential issue. Emergency medications such as rectal diazepam may not be perceived as socially acceptable in the school setting (Butler et al, 2020).
In order to bypass hepatic first pass metabolism, mucosal administration may be considered, through the oral/buccal or nasal mucosa. The bioavailability of midazolam, for example, is 57% when given intranasally, compared to 30% when administered orally (Skinner, 2008) and is seen as an effective sedative in children (Mayel et al, 2020), as well as dexmedetomidine (Mason and Lerman, 2011). Fentanyl and ketamine provide effective analgesia via this route, with the benefit of no histamine release, avoiding nasal itching and congestion in ketamine (Pansini et al, 2021). ‘Dripping’ the medication into the nose is the most basic method of administration, but a compliant child is needed, so often, the mucosal atomizer is used (Sorrentino, 2015).
Absorption of inhaled drugs for the lungs (for example, inhaled or nebulised salbutamol for asthma) might be more dependent on technique rather than physiology (Jones, 2022), such as smaller respiratory tracts and lower inhalation flow rates (Kwok and Chan, 2014).
Considering developmental changes is also important when considering topical medications: absorption may be higher in newborns and babies due to enhanced hydration of the epidermis, enhanced perfusion of the subcutaneous layer of the skin, and also the larger total body surface area ratio, in comparison to adults (Lu and Rosenbaum, 2014). Caution also needs to be taken in alcohol-based preparations and topical corticosteroids, as this can result in toxic effects.
Intramuscular injections obviously have a high bioavailability, but due to the pain these should be avoided where possible in children (Skinner, 2008). Absorption may also be delayed in neonates due to the reduced blood flow to their skeletal muscles (Lu and Rosenbaum, 2014). If given intravenously (IV), drugs are directly entering the systemic circulation: IV administration is the preferred route for severely ill neonates, but care must be taken regarding fluid volumes. Placement of lines is also challenging (Linakis et al, 2016). Administration of medications overcome a variety of barriers prior to optimal absorption (Sage et al, 2014). An understanding of developmental changes during rapid growth in infancy and childhood is imperative, as it is evident that this can affect the pharmacokinetics of different medications (O'Hara, 2016).
This first A–Z article has demonstrated an insight into the various aspects that need to be considered in absorption in neonates and children.


